Medical centers willing to perform liver transplants for severe alcoholic hepatitis patients without the six-month abstinence period, reveals a recent study.
‘Liver transplant centers enabling potentially life-saving liver transplantation for patients with severe alcoholic hepatitis, even before they stop drinking alcohol.’





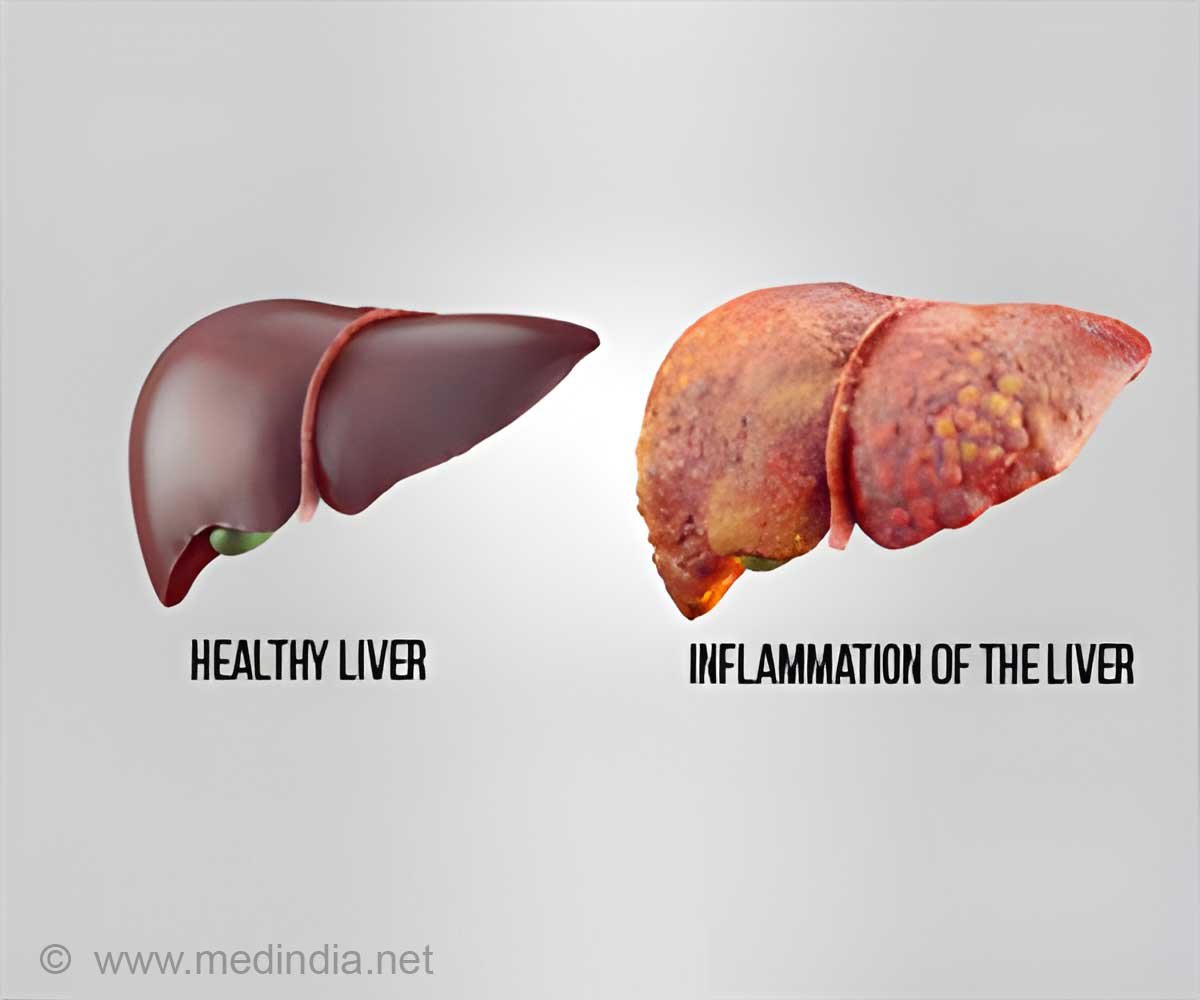
"Liver transplant for severe alcoholic hepatitis is being increasingly accepted, with positive outcomes, and the hope is that more and more patients will be evaluated for transplants," said Saroja Bangaru, MD, chief resident in internal medicine at the University of Texas Southwestern Medical Center, Dallas, and co-author of the study. "The hope is that survival rates are encouraging enough for centers, so that even more of them will reverse past practices."Severe alcoholic hepatitis has an extremely high mortality rate. The primary treatment option has been the use of steroids, predominantly prednisolone. But, many patients do not respond to steroids, and a significant percentage of them will die within three months.
Historically, centers would not perform transplants until patients had stopped drinking for six months due to concerns about a return to drinking after transplant. Additionally, there was a perceived high risk that patient's continued drinking would cause them to miss medical appointments and failure to take their immunosuppressant medications, which prevent organ rejection, all of which could contribute to transplant failure.
Only in recent years have limited studies begun to show greater success for transplants for severe alcoholic hepatitis, Bangaru said. These studies have also shown that a variety of other factors -- aside from recent drinking -- influence whether a patient relapses. These include whether the patient has good social support, suffers from psychiatric ailments and accepts that they have an alcohol problem. "These studies suggest that predicting risk of relapse is much more complicated than just duration of abstinence," Bangaru said.
Study design and results
Advertisement
The survey found that centers have become more willing to perform transplants, as long as patients are carefully screened. Researchers reported that centers use highly selective criteria in approving candidates for transplant, assessing their medical history, social support system and whether they have additional health problems, particularly psychiatric disorders.
Advertisement
The survey also concluded that most transplant centers had "inadequate" post-transplant support for patients. While most offered the services of social workers, only a limited number provided psychiatric or group therapy support that could be very important in helping patients avoid relapse and further medical problems.
Next steps
Dr. Bangaru said further study is needed to encourage more transplants, in particular a controlled clinical trial that follows survival rates over one, three and five years, along with an assessment of rates of alcoholic relapse.
Source-Eurekalert