Breakthrough in tissue engineering as 'shape memory' supports tissue growth.
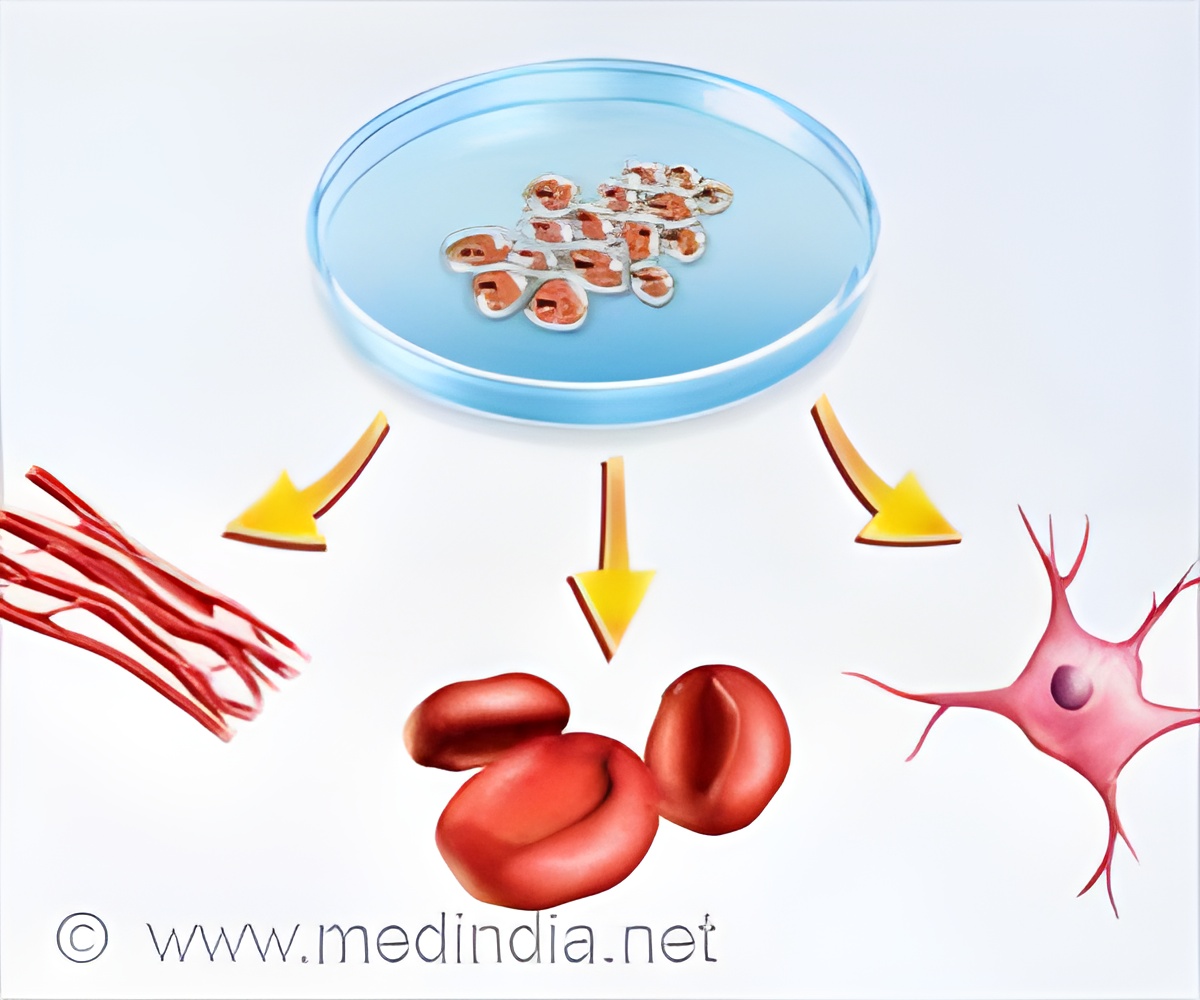
‘Viability of 3D-printed tissue scaffolds has been demonstrated to harmlessly degrade while promoting tissue regeneration following implantation. This breakthrough in tissue enginViability of 3D-printed tissue scaffolds has been demonstrated to harmlessly degrade while promoting tissue regeneration following implantation. This breakthrough of scaffolds 'shape memory' in tissue engineering may enable further research for improved treatment outcomes among patients.
’





"The scaffolds have evenly distributed and interconnected pores that allow diffusion of nutrients from surrounding tissues. The shape memory means this structure is retained when the scaffold is implanted into tissues, and this supports the infiltration of cells into the scaffold while encouraging tissue regeneration and revascularization," says Professor Andrew Dove, from the University of Birmingham's School of Chemistry, who led the research group. The 3D Scaffold
The researchers created the scaffolds using 3D printing resin 'inks' (4Degra™ resins) that has several major advantages like sufficient elasticity to conform to irregular spaces, the ability to undergo compression of up to 85% before returning to their original geometry, compatibility with tissues, and non-toxic biodegradation.
The scaffold structure allows for slow, continuous tissue infiltration. The results were validated in a mouse model that simulates implantation into adipose (fat) tissue. This technique is far superior to current approaches used to fill soft tissue voids that remain after trauma or surgery.
"We have demonstrated that it's possible to produce highly porous scaffolds with shape memory, and our processes and materials will enable the production of self-fitting scaffolds that take on soft tissue void geometry in a minimally invasive surgery without deforming or applying pressure to the surrounding tissues. Over time, the scaffold erodes with minimal swelling, allowing slow continuous tissue infiltration without mechanical degradation," says, Professor Dove.
Advertisement
Source-Medindia