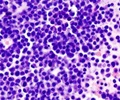
Genomic alterations in pediatric relapsed acute lymphoblastic leukemia have been identified by researchers.

‘Genomic alterations in pediatric relapsed acute lymphoblastic leukemia that cause both therapy resistance and improved clinical response to multi-agent chemotherapy treatment have been identified by researchers.’





Q: Why is this topic important to explore?A: Treating patients with a combination of multiple drugs has allowed 95% of pediatric cases to go into remission, and 80% of those can remain leukemia free. However, patients who experience disease relapse or those who do not respond to drug therapy have very poor prognoses. Although some genetic markers are found to be associated with ALL relapse, not enough is known about the overall genetic makeup of relapsed ALL; nor are the causes of drug resistance understood.
Q: How did you approach this work and what did you discover?
A: In order to explore common mutations that occur in relapsed ALL, we utilized state-of-the-art sequencing technologies to examine the DNA alteration in 55 pediatric relapsed ALL cases. Through these advanced experimental and computational investigative methods we were able to identify specific genomic changes and validate our findings in 279 additional samples. We found that ALL relapse emerges from small, often clinically undetectable populations of cancer cells that are only partially genetically similar to the dominant leukemic population at diagnosis. We also identified numerous new mutations in genes involved in drug resistance that are specific to relapsed ALL. In particular, we showed that mutations in the RAS family of genes cause resistance to methotrexate, a drug commonly used in combination with others to treat ALL; however, these same mutations improved cancer response to another ALL treatment drug, vincristine.
Q: What is the implication of these findings?
A: These results highlight how drug therapy can impact the evolution of leukemia, and show a previously unrecognized role of RAS mutations as causes of both sensitivity and resistance to chemotherapy. Early identification of these mutations, as well as other genetic alterations that have been shown to induce therapeutic resistance in leukemia patients is pertinent in guiding precision medicine treatment strategies and prevention of relapsed disease; a goal that is now being perused in my lab at Rutgers.
Source-Newswise