New research suggests shingles vaccine may be given to patients taking biologics for auto-immune diseases such as rheumatoid arthritis without increasing the risk of adverse reaction to the vaccine.

"The vaccine is a live attenuated vaccine, and the long-standing opinion in the medical community is that patients with certain immune-related diseases receiving immunosuppressive therapies like biologics are at increased risk of contracting varicella from the vaccine itself," said Jeffrey Curtis, M.D., lead author of the study and associate professor in the division of Clinical Immunology and Rheumatology in UAB''s School of Medicine. "However, that opinion has not been definitively bolstered by scientific studies."
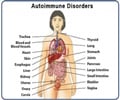
Curtis and fellow researchers examined 463,541 Medicare patients 60 years and older with five immune-related conditions: rheumatoid arthritis, psoriasis, psoriatic arthritis, ankylosing spondylitis and inflammatory bowel disease. There were 633 patients who were exposed to biologics at the time of vaccination or within the next 42 days, the time normally associated with potential adverse reactions to a vaccine. Curtis reports that none of the 633 patients developed shingles in that time period.
"While we don''t suggest that there is zero risk, our findings do suggest that the live shingles vaccine may not be associated with an increased risk of contracting varicella or reactivating shingles from the vaccine in this population," said Curtis. "Our data call into question the current recommendations from the FDA, the Advisory Committee on Immunization Practices and the American College of Rheumatology that the shingles vaccine is contraindicated in patients receiving biologics."
Curtis also said the study re-affirmed the vaccines'' efficacy in preventing shingles in both healthy adults and those with immune-related conditions. He said that in healthy individuals over 60, the vaccine was very effective and cut the risk of contracting shingles by half. Those with immune-related conditions had a similar decrease in risk of developing shingles within the next two years following vaccination.
"We''ve long known that patients with immune-mediated disease are at increased risk for shingles after age 60, yet this study showed that only about five percent of these patients get the vaccine, possibly due to perceived safety concerns," said Curtis. "Our findings suggest the vaccine is effective in this population, and the risk of developing the disease as a direct result of being inoculated with the vaccine may not be significant enough to require a contraindication for its use among patients receiving biologic therapies, including anti-TNF medications like etanercept, adalimumab, infliximab, certolizumab and golimumab."
Advertisement
Collaborators on the study from UAB were Jie Zhang, Ph.D., Fenglong Xie, MS, Elizabeth Delzell, ScD., Lang Chen, Ph.D., Kenneth Saag, M.D., and John Baddley, M.D., along with Kevin Winthrop, M.D., Ph.D., Oregon Health and Science University and James Lewis, M.D., University of Pennsylvania.
Advertisement
Source-Newswise