According to a recent study, reminding primary care doctors to test at-risk patients for osteoporosis can prevent fractures and reduce health care costs.
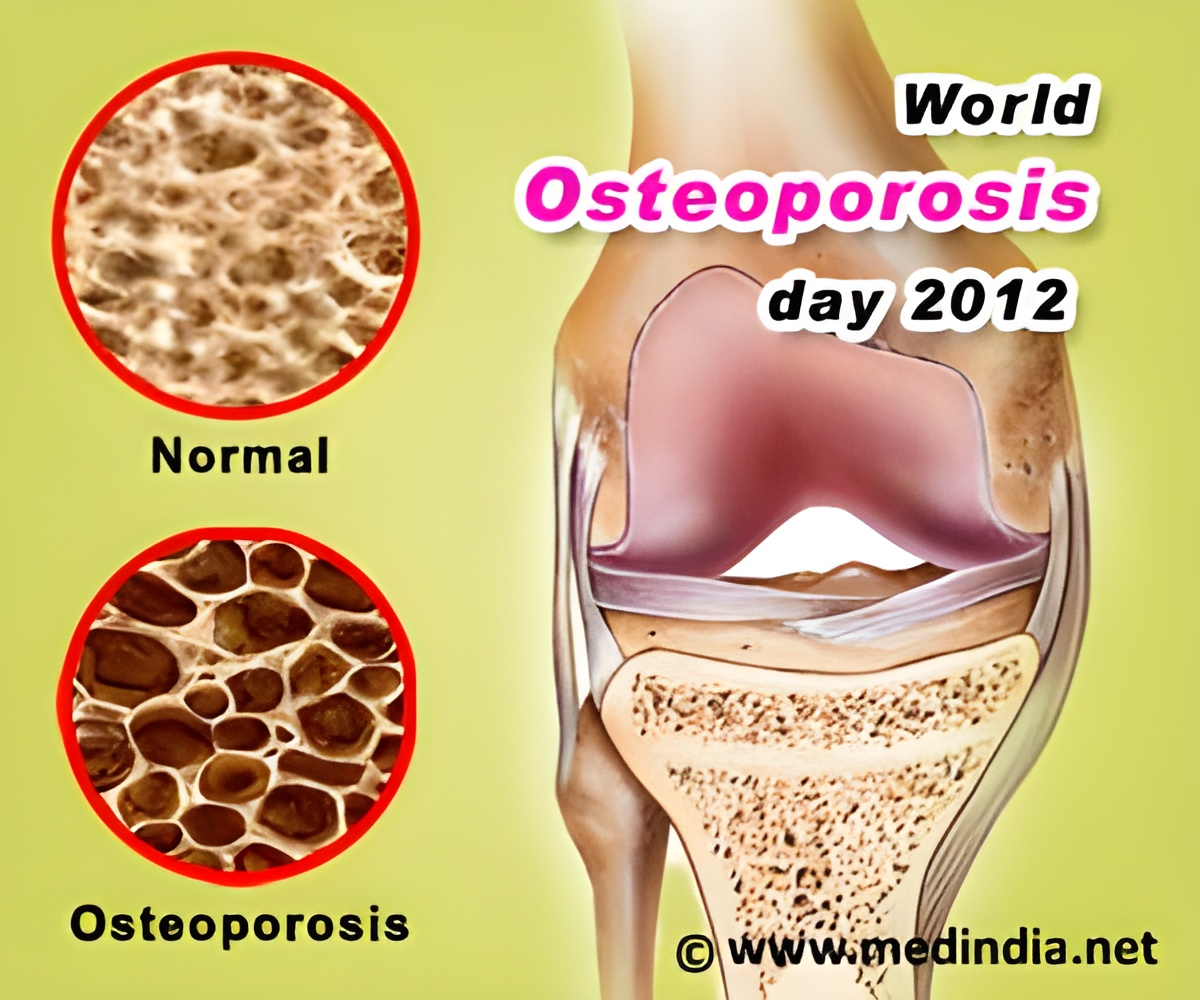
Osteoporosis is a condition that is common, costly and undertreated. Low trauma fractures in older individuals are a "red flag" for osteoporosis, but those at risk often are not treated for the condition. Rates of osteoporosis testing and treatment are typically less than 20 percent in the first year after a fracture.
"Sending family doctors and patients a reminder letter about evaluating fracture patients for osteoporosis significantly improved care at a very low cost," said William D. Leslie, MD, MSc, of the University of Manitoba in Canada, and senior author of this study. "The procedure more than paid for itself – in the long term it is projected to prevent fractures and save money."
The intervention involved two mail-based notices, one sent just to the physicians of more than 4,000 patients with recent fractures, and the other sent to both physicians and patients. The notices to physicians were personalized letters that included bone mineral density (BMD) testing guidelines and a flowchart of osteoporosis management. The second intervention combined the physician letter with a personalized letter to patients acknowledging their recent fracture and recommending they see their primary care physician for an osteoporosis assessment.
These mail notices were inexpensive but effective. The notice to physicians cost just $7.12 (Canadian) per patient, and the note to physicians and patients cost $8.45. Within one year osteoporosis treatments increased by 1.5-fold (4 percent) as a result of the physician letter, and the physician-patient outreach increased treatment rates by 1.8-fold (6 percent) in the same time span. Economic simulations showed that for every 1,000 patients who received physician intervention, there were two fewer fractures, two more quality-adjusted years of life gained and $18,000 saved.
"Simple educational strategies targeting doctors and patients after a fracture have consistently failed to improve the quality of osteoporosis care," said Leslie. "The emergency doctors and orthopedic surgeons who treat fractures are not the ones responsible for preventing the next fracture – and the family physicians who deal with prevention aren't usually part of the team that treats the fracture. Connecting everyone involved – specialists, family physicians and patients – systematically allowed for better care. A simple and very low-cost system using reminder letters can contribute to addressing this 'care gap' and is a strategy that would be easy for others to adopt."
Advertisement