According to scientists, a molecule involved in asthma and allergies has now been shown to make mice resistant to skin cancer.

"But at extremely high levels, TSLP appears to train the immune system to recognize skin cancer cells, and target those cells for elimination," says Raphael Kopan, PhD, the Alan A. and Edith L. Wolff Professor of Developmental Biology. "These experiments demonstrate that there is a way for a natural molecule to help immune cells recognize and reject tumors, at least in the skin."
The study appears online Oct 15 in Cancer Cell.
These findings are surprising because most current evidence suggests that the allergic inflammation and release of TSLP increases -- not decreases -- the risk of tumor development.
The disparity may be explained by the amount of TSLP that is produced. The mice that were resistant to skin tumor growth had blood levels of TSLP that were 1,000-fold higher than normal. And levels in the skin -- where it is made -- may be even higher.
"This is an example of where hyper-vigilance of the immune system may end up paying dividends," Kopan says. "Not only does it respond aggressively to an innocuous allergen, but it begins to monitor, survey and destroy cells that are mutant."
Advertisement
For Kopan’s group, the new research is the culmination of work that began more than six years ago. He and then graduate student Shadmehr Demehri, MD, PhD, wanted to investigate the defects found in mice born without a certain signaling protein in the skin. The protein, called Notch, is vital in properly forming many of the body’s tissues, including skin.
Advertisement
"We were just trying to understand what was going on with our mice," Kopan says. "We did not set out to find a way to stimulate the immune system to eradicate tumors. But it’s often the unexpected observations that lead to practical outcomes."
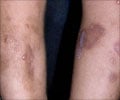
Since the mice expressed elevated levels of TSLP for genetic reasons related to abnormal Notch signaling, Kopan, Demehri and their colleagues asked whether TSLP would likewise protect normal mice from skin cancer. They tested a drug called Calcipotriol that dermatologists prescribe to treat psoriasis. Calcipotriol is considered a vitamin D "mimic" and is known to cause the skin to produce TSLP.
The researchers found that applying Calcipotriol to the skin of normal, healthy mice protected them from developing skin tumors when exposed to cancer-causing agents. In addition, they saw that existing skin tumors in otherwise normal mice shrank when Calcipotriol was applied.
"We already have treatments in clinical practice, often for other conditions, that induce the skin to produce TSLP," says Demehri, now a dermatology resident who treats patients at Barnes-Jewish Hospital. "So the next step is to find out if these topical drugs will be helpful in treating pre-cancerous skin lesions in humans."
Kopan stresses that more work must be done to fully understand the role of TSLP in skin cancer. In particular, these short-term studies were limited to the skin of mice and could not completely explain why Calcipotriol protected the healthy mice from skin cancer.
"In the Calcipotriol experiments, we have not fully separated whether the drug’s beneficial effects are due to the production of TSLP, or the fact that the drug mimics vitamin D," Kopan says.
According to Kopan, future studies will also investigate whether TSLP might have similar effects on other types of cancer.
Demehri S, Turkoz A, Manivasagam S, Yockey LJ, Turkoz M, Kopan R. Elevated epidermal thymic stromal lymphopoietin levels establish an anti-tumor environment in the skin. Cancer Cell. Online Oct. 15, 2012.
Di Piazza M, Nowell C, Koch U, Durham A-D, Radtke F. Loss of cutaneous TSLP dependent immune responses skews the balance of inflammation from tumor-protective to tumor-promoting. Cancer Cell. Online Oct. 15, 2012.
Demehri S, Morimoto M, Holtzman MJ, Kopan R. Skin-derived TSLP triggers progression from epidermal-barrier defects to asthma. PLoS Biology. May 19, 2009.
The work was supported by grants from the National Institute of General Medical Sciences (GM55479-16), the American Asthma Foundation and the National Institutes of Health (NIH) (2 U19 AI070489-09 and P30 CA091842).
Washington University School of Medicine’s 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children’’s hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked sixth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children’s hospitals, the School of Medicine is linked to BJC HealthCare.
Source-Newswise