Exposure to UV radiation is the major cause of skin cancer. Screening the hyperhotspots could offer a new means of predicting a person's skin cancer risk.
‘High-risk individuals could be watched closely by a dermatologist so that skin cancers are detected early.’
Read More..




The study was published in the November edition of Proceedings of the National Academy of Sciences.
Scientists knew of hotspots, but not of ultra-sensitive hotspots.Read More..
"These are 100 times more sensitive than other sites in the genome," said Douglas Brash, senior research scientist in therapeutic radiology and dermatology and a member of the Yale Cancer Center. He led the research.
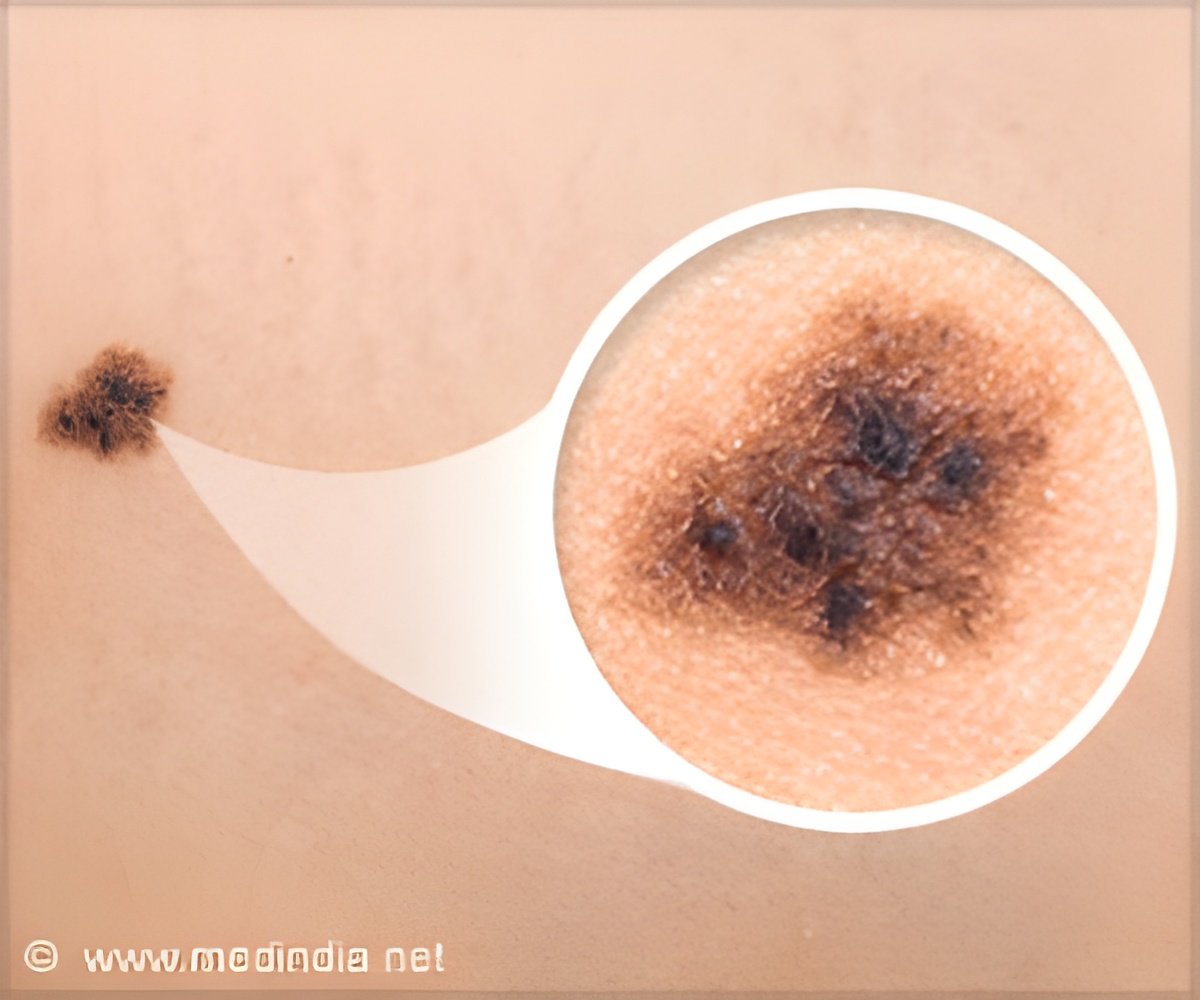
Named "cyclobutane pyrimidine dimer (CPD) hyperhotspots" after the type of DNA damage caused by ultraviolet light, hyperhotspots can be thought of as "bullseyes" that attract damaging radiation. In the study, they occurred most often in melanin-forming cells in human skin known as melanocytes -- the cells in the skin where melanoma skin cancer originates.
"We had thought that DNA damage and mutations that cause cancer were rare events, and random," said Brash. "But this reveals that, at least for skin cancer, there are specific targets in the genome that are waiting to be hit by UV radiation."
To find them, researchers designed a method for tagging sites of CPDs and used high-throughput DNA sequencing to map tags across the genome. They also developed a set of statistical methods for quantifying an individual site's overrepresentation of CPDs relative to the genome average.
Advertisement
The sites where the Yale study identified hyperhotspots are "the same DNA sequences that control the regulation of DNA into RNA and protein, which is how the cell regulates growth," Brash said.
Advertisement
"Why wouldn't evolution want to get rid of these?" Brash said.
The fact that evolution has not eliminated these bullseyes may be a tipoff that the cell uses hyperhotspots for sensing its environment, he said.
The existence of hyperhotspots suggests that mutations spawned by a carcinogen -- UV radiation or other -- are also not entirely random. Mutations related to gene regulation in melanoma tumors were present at CPD hyperhotspots 20,000 times more often than elsewhere.
The Yale study suggests new ways of assessing skin cancer risk, said the researchers.
The most important factor for evaluating the risk is prior UV exposure. But doctors currently lack an objective means of measuring it, relying typically on patients' memories of former sunburns. If doctors could take a small skin sample and examine the hyperhotspots, Brash said, they could get a true picture of the DNA damage from prior sunburn at these sites and have a much better understanding of a patient's exposure history and skin cancer risk.
High-risk individuals could be watched closely by a dermatologist so that skin cancers are detected early, when they are still curable.
Source-Eurekalert














