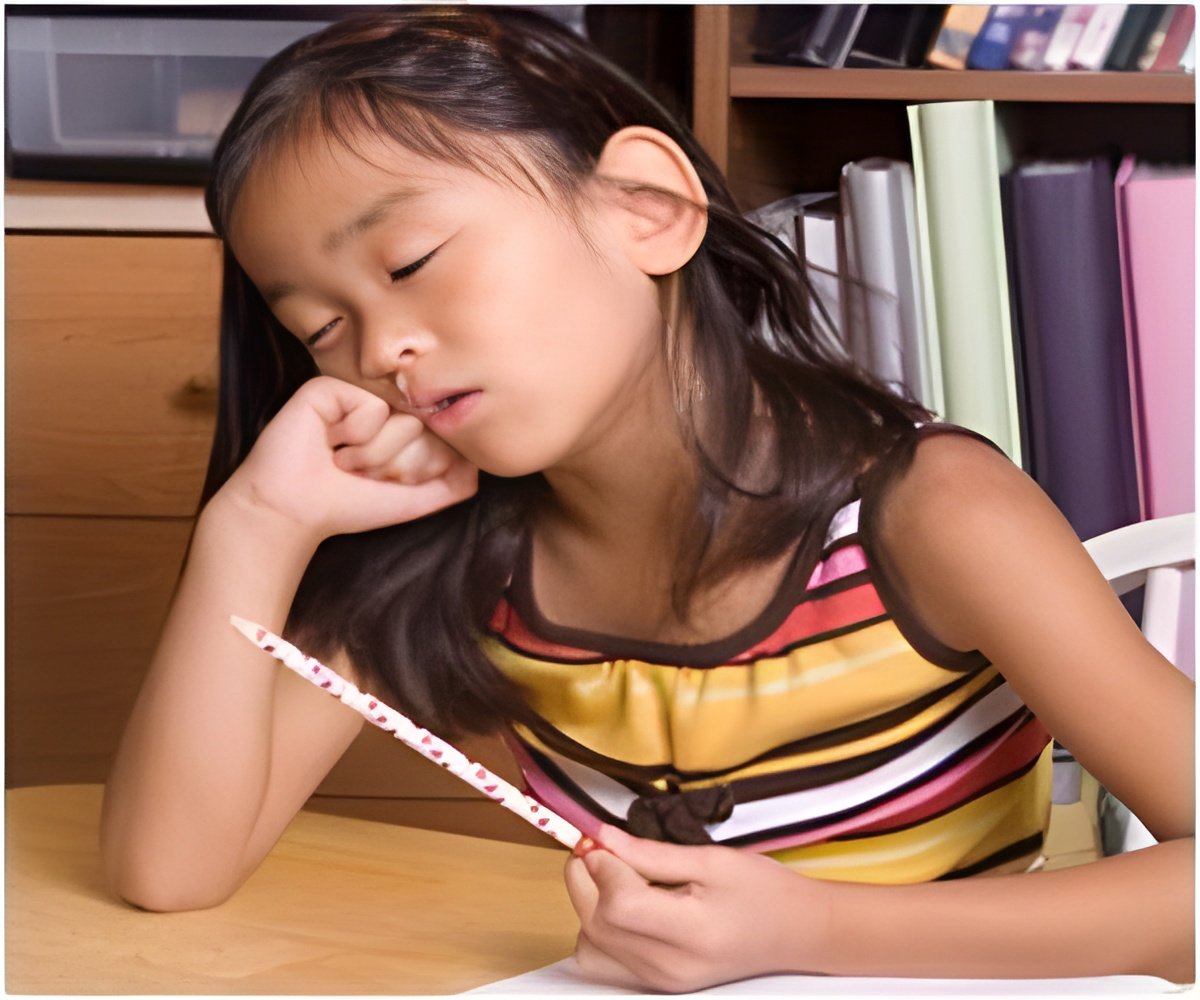
A recent study establishes a link between sleep-disordered breathing and increased risk for behavioral problems in children.
When their children were approximately four and seven years old, parents filled out the Strengths and Difficulties Questionnaire (SDQ), which is widely used to assess behavior. The SDQ has scales for assessing a child's inattention/hyperactivity, emotional symptoms (anxiety and depression), peer problems, conduct problems (aggressiveness and rule-breaking), and prosocial behavior (sharing, helpfulness, etc.). The researchers controlled for 15 potential confounding variables, including socioeconomic status, maternal smoking during the first trimester of pregnancy, and low birthweight.
"We found that children with sleep-disordered breathing were from 40 to 100 percent more likely to develop neurobehavioral problems by age 7, compared with children without breathing problems," said Dr. Bonuck. "The biggest increase was in hyperactivity, but we saw significant increases across all five behavioral measures."
Children whose symptoms peaked early—at 6 or 18 months—were 40 percent and 50 percent more likely, respectively, to experience behavioral problems at age 7 compared with normally-breathing children. Children with the most serious behavioral problems were those with SDB symptoms that persisted throughout the evaluation period and became most severe at 30 months.
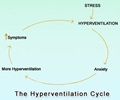
Researchers believe that SDB could cause behavioral problems by affecting the brain in several ways: decreasing oxygen levels and increasing carbon dioxide levels in the prefrontal cortex; interrupting the restorative processes of sleep; and disrupting the balance of various cellular and chemical systems. Behavioral problems resulting from these adverse effects on the brain include impairments in executive functioning (i.e., being able to to pay attention, plan ahead, and organize), the ability to suppress behavior, and the ability to self-regulate emotion and arousal.
"Although snoring and apnea are relatively common in children, pediatricians and family physicians do not routinely check for sleep-disordered breathing," said Dr. Bonuck. "In many cases, the doctor will simply ask parents, 'How is your child sleeping?' Instead, physicians need to specifically ask parents whether their children are experiencing one or more of the symptoms—snoring, mouth breathing or apnea—of SDB."
Advertisement
According to the AAO-HNS, surgery is the first-line treatment for severe pediatric SDB in cases where the tonsils and adenoids are enlarged. Another option is weight loss for overweight or obese children.
Advertisement