Results of a clinical trial that shows how the immune system can engage in fighting HIV infection if given the right boost have been announced by a multi-institutional team of researchers
Wistar's Luis J. Montaner, D.V.M., D.Phil., today presents their findings of the first clinical strategy able to harness host control and decrease HIV reservoir measures, at the 2012 Conference on Retroviruses and Opportunistic Infections in Seattle, Washington. HIV reservoirs are populations of cells that harbor HIV-1, enabling the virus to persist as a chronic infection.
"Our data shows that our human immune response can be made to control HIV in persons who have otherwise lost that ability and, if sustained by natural interferon production, it establishes proof-of-concept that a functional cure is theoretically possible," said Montaner, a professor at Wistar and director of the Institute's HIV-1 Immunopathogenesis Laboratory. "And while we still have much to pursue with this early clinical finding, I firmly believe this gives us hope that one day we can control—and eventually eradicate—HIV in absence of antiretroviral therapy."
The trial showed that interferon-alpha when used as a drug (Peg-IFN-α2A) sustained control of HIV in 9 of 20 patients while also decreasing measures of HIV reservoirs in patients otherwise dependent on antiretroviral therapy (ART). No other clinical strategy to date has shown an impact on decreasing integrated HIV DNA levels in HIV-infected humans.
"While our data may not immediately change clinical practice, it identifies the first strategy that shows a clinical response where both viral replication and HIV reservoir indicators are observed to be reduced in absence of current chemotherapy," Montaner said. "This is the type of response HIV cure research aims to achieve."
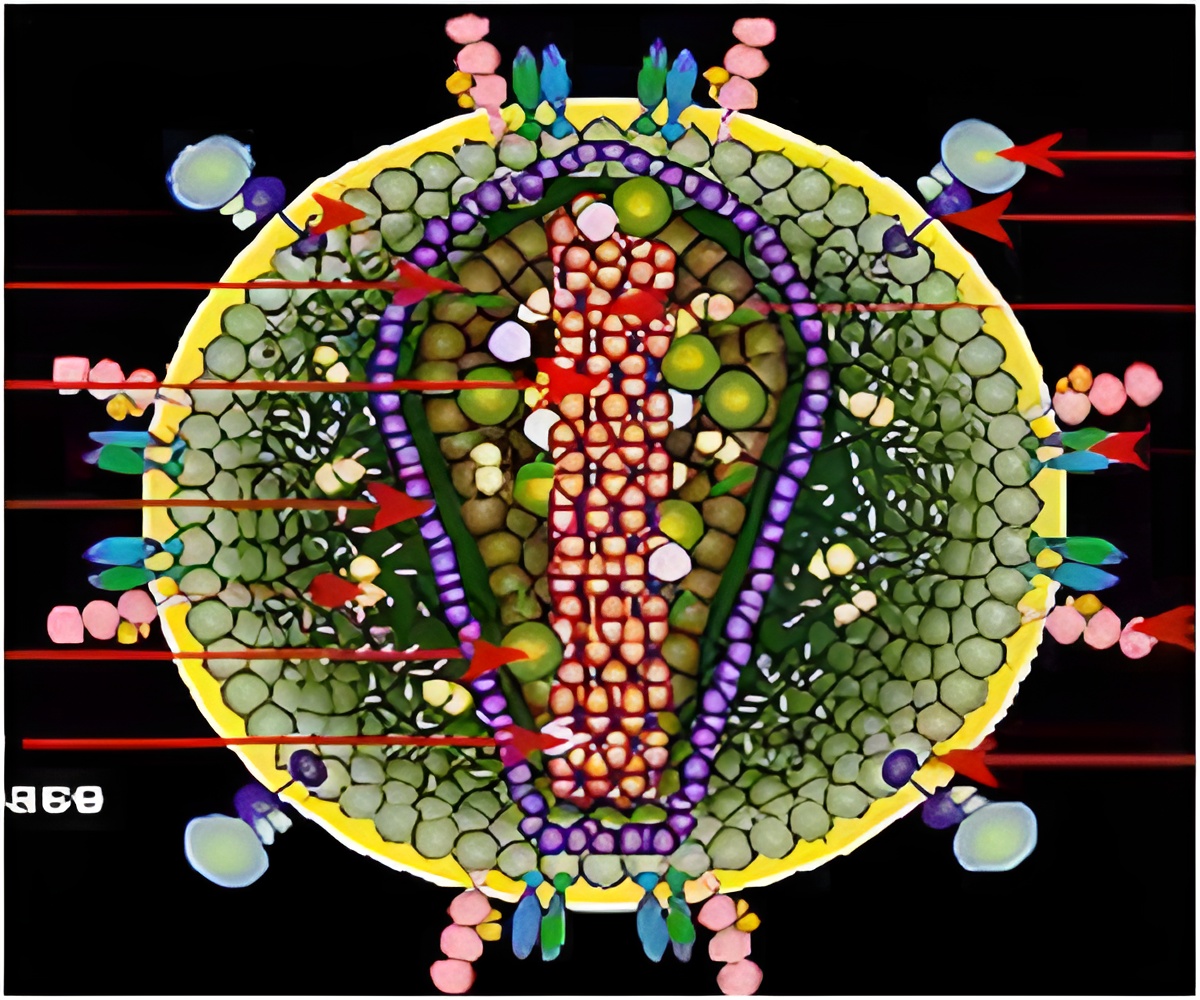
The study analyzed 20 patients over a period of 24 weeks. Remarkably, 45 percent of these patients were able to sustain viral control under 400 copies per mililiter and a similar frequency showed more than 50 percent reduction in circulating HIV reservoirs, as measured by the laboratory of Una O'Doherty, M.D., at the University of Pennsylvania. According to the researchers, these results show that our immune system, which is targeted by the HIV-1 virus, can mount a defense to HIV infection, if given the right stimulation.
Advertisement
"When someone is first infected with HIV-1, the immune system is overwhelmed, and the natural release of interferon into the bloodstream is ineffective as cells that produce it are quickly impaired," Montaner said. "But in our study, conducted at a later stage of chronic infection in an individual, we saw that adding interferon to a recovered immune system can have a dramatic effect in directing responses against HIV-1 to both control and reduce its detection within places we know it can hide."
Advertisement
"It is exciting to show control against HIV-1 can be regained by way of stimulating natural mechanisms," Montaner said. "Our findings also open the way to determine if we can move this clinical research strategy towards a cure based on the decrease in HIV reservoirs we observed."
Interferon-alpha is a chemical naturally manufactured by the human immune system to "interfere" with the ability of viruses to replicate within cells. Since human interferon does not persist long enough in the body to serve as a useful antiviral drug, pharmaceutical researchers modified it by adding polyethelyne glycol (PEG) to the interferon molecule, making it last longer in the bloodstream with less toxicity. This "pegylated" form of interferon was approved in 2008 to treat hepatitis B and C infections.
Source-Eurekalert









