New research published online in the cancer journal, Annals of Oncology says that intrauterine devices can also be used to treat and cure cancer of the endometrium.

Endometrial cancer is the sixth most common cancer in women worldwide. In 2008 there were an estimated 287,630 cases diagnosed in the world, accounting for 4.8% of all female cancers, and 74,170 deaths (2.2% of all female deaths from cancer) [2]. The usual treatment is a total hysterectomy with the removal of the womb and ovaries, but this results in the end of the woman's fertility. Sometimes it is possible for patients to be given oral hormone therapy to slow down the growth of the cancer, but systemic hormone therapy can have adverse side effects such as allergic skin rashes, nausea and vomiting, headaches and abnormal uterine bleeding.
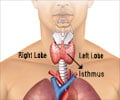
Now, a team of researchers in Italy has conducted the first prospective clinical trial to see whether an intrauterine device (IUD) releasing the progestin hormone levonorgestrel [3], combined with a monthly injection of gonadotropin-releasing hormone (GnRH) for six months could halt and reverse the cancer's growth in women aged 40 or younger. Intrauterine levonorgestrel inhibits growth of the endometrial layer of the womb, while GnRH stops the production of oestrogen, which is the hormone that promotes the development of endometrial cancer.
Women were only eligible for the study if they had atypical endometrial hyperplasia (AEH) – a precursor of endometrial cancer – or early cancer that had not spread and that was confined to the inner layer of the womb, the endometrium. Between 1996 and 2009, 39 patients, aged between 20 and 40, were treated at the European Institute of Oncology in Milan, with results from a total of 34 being available for analysis in this paper.
The IUD was left in place for a year, and then, as long as the cancer had not continued to grow or had recurred, it was removed, enabling the women to plan for pregnancies. After the IUDs were removed, the doctors followed up the women every six months to check that cancer had not returned. Once the women had completed their desired number of pregnancies, they had hysterectomies in order to ensure the cancer was unable to recur in the longer term. Some women who were very young when diagnosed with cancer were able to become pregnant several years after their IUD treatment.
Of the 20 patients with AEH, 19 of them (95%) had a complete initial response to the treatment, although four relapsed later and had to be re-treated. Of the 14 patients with early stage endometrial cancer, 8 (57.1%) had a complete response, and the disease progressed in four women (28%). Two patients with initial complete response experienced relapse. After treatment of any relapses or recurrences, either by further IUD and GnRH treatment, or, where necessary, by hysterectomy, all the women are still alive without evidence of disease. Nine women achieved 11 spontaneous pregnancies and nine babies have been born.
Advertisement
In addition to being used as a contraceptive, the levonorgestrel IUD has become doctors' first choice for treating endometriosis and dysfunctional bleeding. This trial suggests it can now be used for treating specific types of endometrial cancer as well.
Advertisement
He said that levonorgestrel-releasing IUDs could be used for treating AEH and early endometrial cancer now, as long as patients were carefully selected and evaluated using laparoscopy, ultrasound and MRI in order to be certain that their cancer had not spread and that there was no concomitant ovarian cancer, which is more likely in women with endometrial cancer. In addition, the women should be treated in specialist cancer centres, ideally more than one pathologist should check that a correct diagnosis was being made, and the women should be followed up closely, even after completing their childbearing.
"The results of this trial give encouragement for starting a multi-centre, international trial in order to elucidate the best approach for women with endometrial cancers who wish to become pregnant. We need to know which option of treatment is better in terms of efficacy and adverse effects," said Dr Minig.
"The results also open a new area of research into the possibility of carrying drugs (in this case it was progesterone) directly into an organ (in this case, the uterus). For instance, for uterine disease, it might be possible to use an IUD to deliver chemotherapy or other active drugs directly into the uterus, even in menopausal patients, to cure early endometrial cancer and to avoid surgery."
Source-Eurekalert