A study among a large population of Medicare beneficiaries identified patients with heart failure who benefited from implantation of a cardiac resynchronization therapy defibrillator.

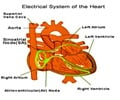
"Clinical trials have shown that cardiac resynchronization therapy (CRT) improves symptoms and reduces mortality and readmission among selected patients with heart failure and left ventricular systolic dysfunction. Following broad implementation of CRT, it was recognized that one-third to one-half of patients receiving the therapy for heart failure do not improve. Identification of patients likely to benefit from CRT is particularly important, because CRT defibrillator (CRT-D) implantation is expensive, invasive, and associated with important procedural risks. A primary question regarding optimal patient selection for CRT is whether patients with longer QRS duration or left bundle-branch block (LBBB) morphology derive greater benefit than others," according to background information in the article. QRS duration is a measurement of the electrical conducting time of the heart on an electrocardiogram. Left bundle-branch block is a cardiac conduction abnormality.
Pamela N. Peterson, M.D., M.S.P.H., of Denver Health Medical Center, Denver, and colleagues conducted a study to determine the long-term outcomes of patients undergoing CRT-D implantation and associations between combinations of QRS duration and presence of LBBB and outcomes, including all-cause mortality; all-cause, cardiovascular, and heart failure readmission; and complications. The study included Medicare beneficiaries in the National Cardiovascular Data Registry's ICD Registry between 2006 and 2009 who underwent CRT-D implantation. Patients were stratified according to whether they were admitted for CRT-D implantation or for another reason, then categorized as having either LBBB or no LBBB and QRS duration of either 150 ms or greater or 120 to 149 ms. Patients underwent follow-up for up to 3 years, through December 2011.
Mortality rates in the primary overall study cohort were 0.8 percent at 30 days, 9.2 percent at 1 year, and 25.9 percent at 3 years. Rates of all-cause readmission were 10.2 percent at 30 days and 43.3 percent at 1 year. The researchers found that after adjustment for demographic and clinical factors, compared with patients with LBBB and QRS duration of 150 ms or greater, the other 3 groups had significantly higher risks of mortality and all-cause, cardiovascular, and heart failure readmission. The adjusted risk of 3-year mortality was lowest among patients with LBBB and QRS duration of 150 ms or greater (20.9 percent), compared with LBBB and QRS duration of 120 to 149 ms (26.5 percent), no LBBB and QRS duration of 150 ms or greater (30.7 percent), and no LBBB and QRS duration of 120 to 149 ms (32.3 percent). The adjusted risk of l-year all-cause readmission were also lowest among patients with LBBB and QRS duration of 150 ms or greater (38.6 percent), compared with LBBB and QRS duration of 120 to 149 ms (44.8 percent), no LBBB and QRS duration of 150 ms or greater (45.7 percent), and no LBBB and QRS duration of 120 to 149 ms (49.6 percent).
There were no observed associations with complications.
"Although prior data regarding the effects of CRT as a function of QRS duration are largely limited to meta-analyses of clinical trials, this study provides an important perspective on the role of QRS duration in outcomes after CRT implantation in clinical practice," the authors write.
Advertisement
Source-Newswise