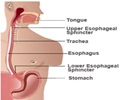
Acute non-variceal gastrointestinal bleeding accounts for approximately 20% of emergency room visits and 5% of admissions.
Acute non-variceal gastrointestinal bleeding accounts for approximately 20% of emergency room visits and 5% of admissions. Although endoscopy has been used as a first-line treatment option in patients with gastrointestinal bleeding, angiographic intervention can be used as a safe diagnostic and treatment method in patients with gastrointestinal bleeding that is refractory to endoscopic treatment. The incidence of rebleeding in patients with negative initial angiography has been reported in up to 60% of cases. However, little is known about the predictive factors for rebleeding.
A research article to be published on August 28, 2009 in the World Journal of Gastroenterology addresses this question. A research team led by Hyo-Cheol Kim from Seoul National University Hospital, Korea, identified the possible predictive factors for rebleeding after negative angiographic findings in patients with acute non-variceal gastrointestinal bleeding.One hundred and twenty eight patients with acute non-variceal gastrointestinal bleeding had negative findings after initial angiography. Clinical and laboratory parameters were analyzed retrospectively.
They found that clinical factors including underlying malignancy, liver cirrhosis, and hematemesis are important predictors for rebleeding after angiographically negative findings in patients with acute non-variceal gastrointestinal bleeding.
Source-Eurekalert
LIN