A family history of breast cancer and dense breast tissue increase the risk of breast cancer for women in their 40s', say researchers.

This research addresses the need for more information about screening women in their 40s—a need that the U.S. Preventive Services Task Force highlighted in its 2009 updated breast cancer screening guidelines. Also published in the Annals of Internal Medicine, these guidelines advise screening mammography every two years for women aged 50 to 74. The guidelines recommend that women in their 40s consider their personal values regarding the benefits and harms and then decide when to begin regular screening.
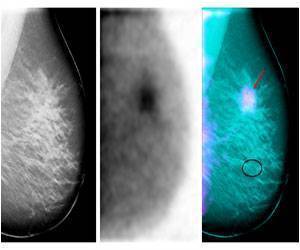
Group Health Research Institute Senior Investigators Diana Miglioretti, PhD, and Diana Buist, PhD, contributed to both of the new Annals articles. Together, the companion articles estimate that the benefits and harms of getting screening mammograms every two years are the same for groups of women aged 40-49 who have a twofold increased risk level of breast cancer as for groups of women aged 50 with an average breast cancer risk level. Factors that increase 40- to 49-year-old women's risk by twofold are having a first-degree relative (parent, sibling, or child) with breast cancer, or having extremely dense breast tissue (as seen on a mammogram).
"Mainly, we wanted to find out the tipping point: what level of increased risk women in their 40s needed to have to reach the same benefit-to-harm ratio for screening mammography as women aged 50 to 74," said Dr. Miglioretti. The international research team used data from the Breast Cancer Surveillance Consortium (BCSC), a U.S. research network of mammography registries. The BCSC is the nation's largest longitudinal collection of breast imaging data, covering 9.5 million mammograms, 2.3 million women, and 114,000 breast cancer cases so far. By continuously collecting information on breast cancer screening, risk factors, and cancer outcomes, the BCSC provides long-term data on screening as it occurs in everyday clinical practice to help answer preventive health care questions.
Tipping the balance of benefits and harms to favor screening mammography starting at age 40 years
In one article, Nicolien van Ravesteyn, MSc, Jeanne Mandelblatt, MD, MPH, and colleagues including Drs. Miglioretti and Buist identified the threshold of risk needed for women ages 40 to have comparable benefits and harms as seen when average-risk women aged 50 are screened every other year using mammography. They used four independent well-established simulation models that are part of the National Cancer Institute's Cancer Intervention and Surveillance Modeling Network (CISNET) collaborative. Ms. van Ravesteyn is a researcher at Erasmus Medical Center in Rotterdam, The Netherlands; and Dr. Mandelblatt is the associate director for population sciences at Georgetown University Medical Center's Lombardi Comprehensive Cancer Center in Washington, DC.
Advertisement
"Our population models show what can be expected across populations with different risk levels," Dr. Mandelblatt said. "The models cannot determine outcomes for individual women. Policymakers can use them to inform guidelines for populations."
Advertisement
The first author of the other article is Heidi D. Nelson, MD, MPH, an investigator at the Oregon Evidence-based Practice Center at Oregon Health & Science University and Providence Cancer Center in Portland. With Drs. Buist and Miglioretti and colleagues including Ellen O'Meara, PhD, a research associate at Group Health Research Institute, Dr. Nelson conducted a meta-analysis—a rigorous review of previous studies—from 66 publications selected for their relevance and quality. They also conducted new analyses using BCSC data on more than 380,000 women who were 40-49 when they had a screening mammogram from 1994 to 2010, to see how family history and other risk factors affected breast cancer risk for women in their 40s.
Results indicated:
- having a first-degree relative with breast cancer, especially one under age 50, increased risk by more than twofold
- having extremely dense breasts on a mammogram increased risk by more than twofold
- having a previous benign breast biopsy, a second-degree relative with breast cancer, or breast tissue that was heterogeneously dense on a mammogram increased risk between 1.5-fold and twofold.
"Most of the risk factors that we considered did not increase breast cancer risk," Dr. Nelson said. Other potential risk factors that they evaluated—such as race/ethnicity, body mass index, physical activity, and using alcohol, tobacco, or hormone therapy—had effects that were either small, undetectable, or equivocal. "Our results indicate that we can focus on just a few significant risk factors to simplify approaches to risk-based screening for women in their 40s," she added.
The research in the two articles was possible because three national research groups—BCSC, CISNET, and the Evidence-based Practice Center—joined forces. Each contributed unique strengths: extensive data, comprehensive breast cancer models, and data interpretation. The U.S. Preventive Services Task Force previously used information from the three groups to develop its current breast cancer screening recommendations.
In an accompanying editorial, Otis Webb Brawley, MD, chief medical officer and executive vice president of the American Cancer Society and author of the book How We Harm, referred to the BCSC and CISNET as "national treasures."
The authors called for additional research based on the findings, to see how well these risk estimates, which are based on large numbers of women, predict risks for individual women. In the meantime, said Dr. Buist, "taken together, the results from these articles provide strong evidence that professional groups can use to refine screening guidelines."
Source-Eurekalert