Anti-anxiety and anti-psychotic medications prescribed to patients should be monitored closely, as they have a higher tendency to commit suicide.
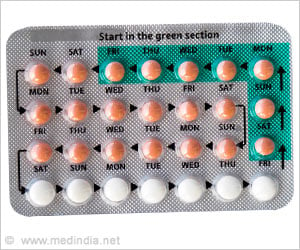
‘Suicidal attempts in patients can be reduced by decreasing the free access to prescribed psychotropics and providing medicines in blister packs.’
Read More..




The study was published in the Journal of Clinical Psychiatry.Read More..
Suicide is the 10th leading cause of death in the nation with 45,000 fatalities in 2016, more than 200,000 hospitalizations and 500,000 emergency department visits.
Survival often depends on the method used and the method usually depends on having physical access to it. Intentional poisoning accounts for 15 percent of all fatal suicides and between 54-68 percent of nonfatal suicide attempts. Drugs make up the vast majority of those poisonings.
The study investigated the association between prescribed access to psychotropic drugs and using them in a suicide attempt. The researchers used a large, nationally representative insurance claims dataset of 27,876 people who had attempted suicide at least once.
They found that 10,158 of them had used psychotropic drugs in their attempt. The most commonly used were anti anxiety medications, followed by antidepressants, antipsychotics or mood stabilizers and stimulants. About 13 percent used more than one drug.
Advertisement
"The most likely options were from family and friends, previous prescriptions filled prior to our exposure period, medications purchased outside of insurance plans or on the black market," the study said.
The findings offer a number of lessons and insights into prescribing these drugs, said the study's senior author Heather Anderson, PhD, associate professor in the Center for Pharmaceutical Outcomes Research at the University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences.
"Restricting or modifying access to psychotropic drugs will require increased attention by all healthcare professionals, particularly pharmacists who are well-positioned to talk to their patients about safe medication use and storage," she said. "It is important to stay on top of a patient's depression, stay on top of their prescriptions and monitor suicidal ideation."
Providing medicine in blister packs has been successful in other countries in reducing deaths because it requires time and effort to remove enough of the drug for an overdose. And people can change their minds during that time.
Ultimately, Brown said, those at high risk for suicide with prescriptions for psychotropic drugs should be closely monitored for potential safety interventions.
### The study co-authors include: Peter M. Gutierrez, PhD; Gary K. Grunwald, PhD; Carolyn DiGuiseppi, MD, PhD; Robert J. Valuck, PhD.
Source-Eurekalert