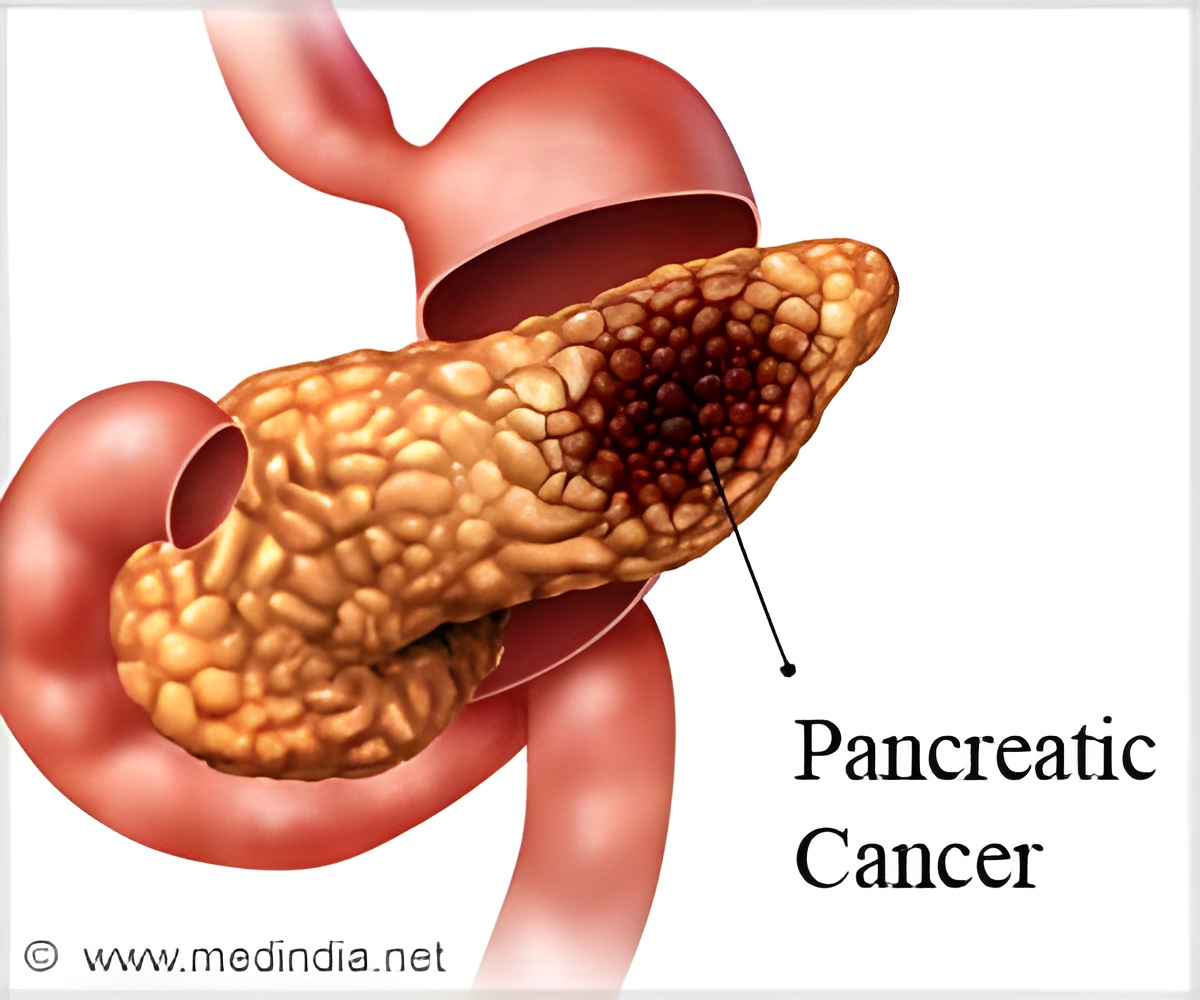
Patients with stage II pancreatic cancer who receive chemotherapy followed by resection live nearly twice as long as patients who receive only chemotherapy.
‘Survival improves in pancreatic cancer patients who receive multimodality therapy, chemotherapy before and/or after resection.’
Read More..




Although chemotherapy can improve outcomes, the risk of surgery is justified because the patients live longer even if the cancerous tissue is not entirely removed, according to the study from researchers at the University of Arizona Department of Surgery, Tucson.Read More..
Surgery can improve survival
The researchers found that patients who received chemotherapy followed by resection lived an average of 19.75 months, while those who received only chemotherapy lived an average of 10.12 months.
They examined data from the National Cancer Database (NCDB), a joint program of the American College of Surgeons and the American Cancer Society.
"Our results show that surgery is viable in more cases than we thought," said Amanda K. Arrington, MD, MHM, FACS, a surgical oncologist at the University of Arizona Department of Surgery, Tucson.
Advertisement
Approximately 10 to 30 percent of these patients present with disease in which resection may be considered an appropriate therapy.
Advertisement
While the goal of resection is to remove all of the tumor tissue, it can be difficult to accomplish, especially if the cancer has spread to nearby blood vessels that feed the liver and small intestine.
Margin status, or how much cancerous tissue is left post-surgery on the edges of the resected area, is a significant predictor of survival after surgery for pancreatic cancer.
Patients with no cancerous tissue left after resection (R0) have improved survival compared with patients with microscopic amounts (R1) or macroscopic amounts (R2) of cancerous tissue left after resection. This study looked at R1 and R2 resection outcomes compared with chemotherapy alone.
Study details
Dr. Arrington and her colleagues searched NCDB data from 2010 to 2015 for stage II pancreatic cancer patients who underwent R1/R2 surgery with or without pre-operational chemotherapy to compare to stage II patients who received chemotherapy alone. They found:
Study results confirm current recommendations for stage II pancreatic cancer, which note that survival improves when patients receive multimodality therapy, chemotherapy before and/or after resection. Further, patients benefit from surgery even in extremely difficult cases that end up with a margin positive resection, Dr. Arrington said.
The researchers found even when the tumor does not shrink significantly in response to chemotherapy, there are still survival benefits to taking an aggressive surgical approach.
"Based on this study, surgeons can be a little more aggressive and offer surgical treatment more often than not to stage II pancreatic cancer patients," Dr. Arrington said. "There are ongoing studies looking at whether more pancreatic cancer patients, including stage I patients, would benefit from surgery after chemotherapy."
Other study authors include Chiu-Hsieh Hsu, PhD; Kenzie L. Schaefer, BS; Catherine L. O'Grady, MPH; Mohammad Khreiss, MD; and Taylor S. Riall, MD, PhD, FACS, all from the University of Arizona.
"FACS" designates that a surgeon is a Fellow of the American College of Surgeons.
Presented at the Western Surgical Association Annual Meeting (virtual), November 2020.
Study authors have no disclosures related to this research.
Source-Eurekalert