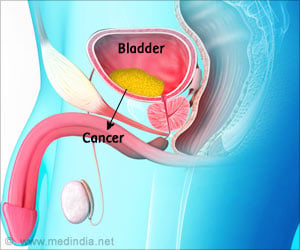
Radical cystectomy is performed in the elderly population where diabetes rates can be high and it is associated with a high incidence of postoperative disease and death.

Using data from the 2002-2009 Nationwide Inpatient Sample database, patients with uncontrolled diabetes undergoing radical cystectomy were compared to those without diabetes undergoing the surgery. Postoperative complications were identified and disposition of patient and length of hospital stay were analyzed. Significant differences in post-surgery outcomes were seen. Patients with uncontrolled diabetes were three times as likely to have post-surgery complications including infection and were three times as likely to die during their initial hospitalization than those patients without diabetes who underwent the same procedure. Results also showed the mean length of hospital stay for the sample with uncontrolled diabetes was 17.3 days compared to 11.4 days for non-diabetic patients.
Senior investigator Robert E. Weiss, MD, Cancer Institute of New Jersey urologic oncologist and professor of surgery at Rutgers Robert Wood Johnson Medical School says the findings demonstrate uncontrollable diabetes can be recognized as a potential modifiable risk factor for this group of patients undergoing this procedure. Along with Dr. Weiss, other authors include Izak Faiena, MD, Viktor Y. Dombrovskiy, MD, PhD, MPH, Raymond C. Sultan, MD, Yana Barbalat, MD, Amirali H. Salmasi, MD, all Robert Wood Johnson Medical School; and Eric A. Singer, MD, MA, Cancer Institute of New Jersey and Robert Wood Johnson Medical School.
Further exploring surgical impacts in the area of genitourinary cancers, Cancer Institute investigators examined data on adrenal cancers. Surgery for this type of cancer, which targets the small glands above the kidneys, is typically done with a traditional open approach. With advances in minimally-invasive methods, investigators wanted to understand how the use of laparoscopic and robotic surgery has changed over time.
Researchers gathered data from the nationally representative Premier Hospital Database on patients who underwent open, laparoscopic or robotic adrenalectomy for cancer between 2003 and 2013. They examined surgeon specialty, patient demographics, hospital characteristics, complications and data pertaining to the immediate period before and after surgery as well as data from the surgery period itself. They found 4,781 surgeries were performed for adrenal cancer - mostly in white males over the age of 50 and more commonly performed by non-urologists (66 versus 34 percent). Among non-urologists, the traditional 'open' method was most commonly performed followed by laparoscopic and robotic approaches (56.3, 37.4 and 6.4 percent respectively) as compared to urologists performing the same approaches (48.8 percent for open method, 38.4 percent for laparoscopic and 12.9 percent for robotic). They found no difference in complication rate or operative time between types of surgeons.
According to senior investigator Eric A. Singer, MD, MA, Cancer Institute of New Jersey urologic oncologist and assistant professor of surgery at Robert Wood Johnson Medical School, the findings show that even though a majority of adrenalectomy cases were performed in the traditional method, minimally-invasive approaches were found to be a safe method for this procedure. Along with Dr. Singer, other authors include Izak Faiena, MD, Alexandra Tabakin, BA, Robert Wood Johnson Medical School; Jeffrey Leow, MD, Brigham and Women's Hospital and Harvard Medical School; Neal Patel, MD, Parth K. Modi, MD, Amirali H. Salmasi, MD, Robert Wood Johnson Medical School; Benjamin I. Chung, MD, Stanford University School of Medicine; and Steven L. Chang, MD, MS, Brigham and Women's Hospital and Harvard Medical School.
Advertisement
"As a National Cancer Institute-designated Comprehensive Cancer Center, Rutgers Cancer Institute of New Jersey is committed to building on this knowledge so that patients may benefit," notes Cancer Institute Director Robert S. DiPaola, MD, a physician scientist who manages the care of prostate cancer patients and is also on this year's Steering Committee for the symposium.
Advertisement