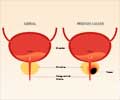
Study says men largely make decisions about prostate cancer screening based on conversations with their clinicians, but these discussions often do not include information about the risks
A report in the September 28 issue of Archives of Internal Medicine, one of the JAMA/Archives journals says that men largely make decisions about prostate cancer screening based on conversations with their clinicians, but these discussions often do not include information about the risks of testing in addition to the benefits.
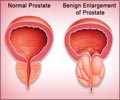
A second report in the same issue uses statistical modeling to estimate the benefits and risks of prostate-specific antigen (PSA) screening in men of various ages and risk levels.The majority of American men older than 50 have been screened with the PSA blood test, according to background information in one of the articles. However, the practice is controversial because there is no convincing evidence that screening prevents deaths from the disease, and treating early-stage cancers detected by screenings may lead to important complications. "Given the uncertain benefit for screening and known treatment risks, prostate cancer screening decisions should be guided by patient preferences," the authors write. "Indeed, most professional organizations recommend that the first step in screening should be a discussion between health care providers and patients about the risks and benefits of early detection and treatment so that patients can make informed decisions about whether to be screened."
Richard M. Hoffman, M.D., M.P.H., of New Mexico VA Health Care System and University of New Mexico School of Medicine, Albuquerque, and colleagues conducted a telephone survey of 3,010 randomly selected English-speaking adults age 40 and older in 2006 and 2007. The sample included 375 men who had either undergone or discussed PSA testing with their clinicians in the previous two years. These men were asked what they knew about prostate cancer, what their discussions with clinicians were like and what factors and sources of information influenced their screening decisions.
Overall, 69.9 percent of the men had discussed screening with their clinician before making a decision, including 14.4 percent who chose not to undergo testing. Most often, clinicians raised the idea of screening (64.6 percent), and 73.4 percent recommended it. Recommendation from a clinician was the only characteristic of the discussion associated with testing.
"Although respondents generally endorsed shared decision-making process and felt informed, only 69.9 percent actually discussed screening before making a testing decision, few subjects [32 percent] reported having discussed the cons of screening, 45.2 percent said they were not asked for their preference about PSA testing and performance on knowledge testing was poor," with only 47.8 percent of men correctly answering any of three questions about prostate cancer risk and screening accuracy, the authors write. "Therefore, these discussions—when held—did not meet criteria for shared decision making. Our findings suggest that patients need a greater level of involvement in screening discussions and to be better informed about prostate cancer screening issues."
In a second study, Kirsten Howard, B.Sc., M.App.Sc., M.P.H., M.Health.Econ., Ph.D., of the University of Sydney, Australia, and colleagues constructed a statistical model to provide information for men age 40, 50, 60 and 70 years at low, moderate and high risk for prostate cancer based on family history. Using Australian prostate cancer incidence rates before PSA screening began in 1989 and cancer death rates in 2005, along with data from the European Randomized Study of Screening for Prostate Cancer and the Australian Bureau of Statistics, the authors examined two hypothetical cohorts of men who either participated in or declined annual PSA screening.
Advertisement
In the model, screened men are two to four times more likely to be diagnosed with prostate cancer than unscreened men, but death rates from prostate cancer and from all causes are not significantly different. This implies that many men whose cancer is detected by PSA screening may be undergoing treatment for clinically insignificant cancers, the authors note.
Advertisement
Editor's Note: Please see the articles for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
Editorial: Study Helps Highlight Difficulties of Shared Decision Making
Virtually every professional organizations' PSA screening guidelines urge clinicians to engage patients in shared decision making before performing PSA testing, write Steven H. Woolf, M.D., M.P.H., of Virginia Commonwealth University, Richmond, and Alex Krist, M.D., M.P.H., in an accompanying editorial.
"Definitions of shared decision making vary, but the term generally refers to the effort to help patients understand the benefits, harms and uncertainties of available options and to apply personal preferences to determine the best choice. Both parties share information, jointly participate in decision making and agree on a course of action that incorporates personal preferences."
"Today's practice environment presents few incentives or support tools for those clinicians and patients who prefer a discussion rather than simply marking a checkbox for PSA on a laboratory requisition form," they continue. "In the United States, where medical technologies are often adopted long before their effectiveness and safety are confirmed, the difficulties of implementing shared decision making for prostate cancer screening will likely recur with other modalities of care. What is ultimately required is a deeper change in culture among providers and consumers of health care to delay dissemination, resist the assumption that newer is better, wait for evidence, tolerate observation over intervention and accept uncertainty."(Arch Intern Med. 2009;169[17]:1557-1559. Available pre-embargo to the media at www.jamamedia.org.)
Editor's Note: Please see the article for additional information, including author contributions and affiliations, financial disclosures, funding and support, etc.
Editorial: Information Can Aid Discussion of PSA Screening
"Data from the National Survey of Medical Decisions reported in this issue of the Archives suggest that many patients have not had an opportunity to discuss the full range of issues related to the PSA screening decision," writes Michael Pignone, M.D., M.P.H., of University of North Carolina–Chapel Hill, in an accompanying editorial.
"Because of the complexity of factors that need to be considered in such discussions, tools have been developed to help guide providers and patients in considering the benefits and downsides of screening and in reaching a value-concordant decision," he continues. "One type of tool, patient decision aids, has been shown to increase patient knowledge, participation and confidence."
"To inform the development of future decision aids, Howard and colleagues present a balance sheet of the consequences of PSA screening in Australian men from different age groups and with different levels of underlying risk," Dr. Pignone continues. "The work by Howard and colleagues is an important step in providing information to patients and providers to facilitate discussion about this trade-off."
Source-Eurekalert
RAS





![Prostate Specific Antigen [PSA] Prostate Specific Antigen [PSA]](https://www.medindia.net/images/common/patientinfo/120_100/prostate-specific-antigen.jpg)