A new study reports that the survival rates in HIV-associated lymphoma patients has stabilized during the antiretroviral therapy (ART) era in the US.

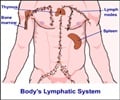
Satish Gopal, M.D., M.P.H., from the Program in Global Oncology at the Lineberger Comprehensive Cancer Center of the University of North Carolina, and colleagues compared differences in presentation and survival, across histologic subtypes and diagnosis years, among HIV-infected lymphoma patients. They also examined predictors of death in this population. Data from 476 HIV-associated lymphoma patients living in the US who were diagnosed with various types of lymphoma including HL, diffuse large B-cell lymphoma (DLBCL), Burkitt lymphoma (BL), primary central nervous system lymphoma (PCNSL), and other types of NHL, between 1996 and 2010 were analyzed using various statistical methods.
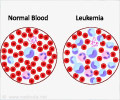
Their results demonstrate that HIV-associated lymphoma is heterogeneous and changing since the ART era began. Clinical presentations across the different lymphoma subtypes was highly variable during the study period (79 HL, 201 DLBCL, 56 BL, 54 PCNSL, and 86 with other NHL). Histologic shifts in the proportion of BL vs other NHL subtypes is increasing consistent with other reports. Data showed that more recently diagnosed patients were older and more likely to be male, of nonwhite/nonblack ethnicity (primarily Latino patients), to be men who have sex with men, and to have prior AIDS-related illness. They were also more likely to be on ART at lymphoma diagnosis with higher CD4 counts and better HIV control. The authors also report that more recent diagnosis year was not associated with decreased mortality and that 61.6% of patients with HIV-associated HL were alive 5 years after lymphoma diagnosis, compared with 50.0% for BL, 44.1% for DLBCL, 43.3% for other NHL, and 22.8% for PCNSL. Of note, lymphomas occurring on ART were associated with a doubling of mortality, which may suggest important biologic differences between tumors developing on and off ART, although these results require confirmation.
Gopal and colleagues conclude, "These results highlight an ongoing need to elucidate lymphoma biology and optimize treatments for this challenging population to reduce deaths from one of the leading causes of mortality in the modern ART era."
In an accompanying editorial, Kieron Dunleavy, M.D., and Wyndham H. Wilson, M.D., Ph.D., from the Metabolism Branch of the Center for Cancer Research at the National Cancer Institute, state the findings reflect the shifting demographics of the HIV epidemic in the US. However, the shift towards more biologically favorable and curable types of lymphoma has not resulted in improved survival over the study period. They assert, "In conclusion, because HIV-associated lymphomas are potentially as curable as those arising in HIV-negative patients, it is critical that they be approached with the same care as HIV negative cases."
Advertisement