Susceptibility of vancomycin strains of S. aureus was not linked to risk of death, finds a study.

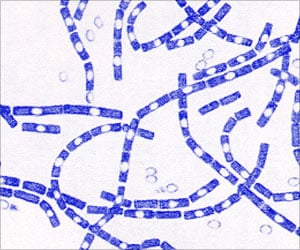
Staphylococcus aureus is among the most common causes of health care-associated infection throughout the world. It causes a wide range of infections, with bloodstream infections (S aureus bacteremia [SAB]) among the most common and lethal. For more than 50 years, the primary therapy for S. aureus infections has been either semisynthetic penicillins or vancomycin. More recent reports have documented an increase in the minimum inhibitory concentration (MIC; the lowest concentration of an antimicrobial agent that inhibits the growth of a microorganism) for vancomycin, referred to as vancomycin "MIC creep" (the development of reduced susceptibility to vancomycin). There have been reports suggesting that elevations in vancomycin MIC values may be associated with increased treatment failure and death, according to background information in the article.
Andre C. Kalil, M.D., M.P.H., of the University of Nebraska Medical Center, Omaha, and colleagues conducted a review and meta-analysis of the evidence regarding the association of vancomycin MIC elevation with mortality in patients with SAB. The researchers identified 38 studies that met criteria for inclusion.
Among 8,291 episodes of SAB included in the studies, overall mortality was 26.1 percent. The adjusted absolute risk of mortality among patients with SAB with high-vancomycin MIC (≥ 1.5 mg/L [less susceptible]; n = 2,740 patients; mortality, 26.8 percent) was not statistically different from patients with SAB with low-vancomycin MIC (< 1.5mg/L; [more susceptible] n = 5,551 patients; mortality, 25.8 percent). In studies that included only methicillin-resistant S. aureus (MRSA) infections (n = 7,232), the mortality among SAB episodes in patients with high-vancomycin MIC was 27.6 percent, compared with a mortality of 27.4 percent among patients with low-vancomycin MIC.
The authors note that the findings cannot definitely exclude an increased risk of death. No significant differences in risk of death were observed in subgroups with high-vancomycin MIC vs low-vancomycin MIC values across different study designs, types of microbiological susceptibility assays, MIC cutoffs, clinical outcomes, duration of bacteremia, previous vancomycin exposure, and treatment with vancomycin.
The researchers write that the findings of this study may have implications for clinical practice and public health, including that standards for vancomycin MIC most likely do not need to be lowered; routine differentiation of MIC values between 1mg/L and 2 mg/L appears unnecessary; and the use of alternative antistaphylococcal agents may not be required for S. aureus isolates with elevated but susceptible vancomycin MIC values. "These conclusions are consistent with current Infectious Disease Society of America treatment guidelines that recommend use of vancomycin for treatment of MRSA bacteremia with consideration for alternative agents based on the patient's clinical response and not the MIC."
Advertisement