New research uncovers how PAG from gut bacteria interacts with adrenergic receptors, impacting heart function and leading to potential advancements in heart failure treatment.

Gut microbe-generated phenylacetylglutamine is an endogenous allosteric modulator of beta 2-adrenergic receptors
Go to source). PAG influences the force of heart muscle contractions by interacting with beta-2 adrenergic receptors, which may contribute to heart failure. Mutations in parts of these receptors, previously thought unrelated to signaling, have been shown to prevent PAG from impairing receptor function in preclinical models.
‘Mutations in beta-2 adrenergic receptors can block the negative effects of Phenylacetylglutamine, offering new hope for heart failure treatments. #medindia #hearthealth
’





This is the latest in a series of investigations into PAG, led by Stanley Hazen, MD, Ph.D, chair of Cardiovascular and Metabolic Sciences in Cleveland Clinic’s Lerner Research Institute and co-section head of Preventive Cardiology. Dr. Hazen’s lab previously demonstrated that elevated circulating levels of PAG in subjects are associated with heightened risk for developing heart failure, and lead to worse outcomes for patients with heart failure. They also showed that the gut microbial PAG signaling pathway was mechanistically linked to numerous heart failure-related features and cardiovascular disease risks. The new findings bring us one step closer to therapeutically targeting this pathway to develop an improved treatment for the prevention of heart failure, Dr. Hazen says.
Role of Beta-Blockers and PAG in Heart Failure
A commonly used heart medication for the treatment of heart failure and blood pressure, called beta-blockers, target our body’s “fight-or-flight" response. This critical response is controlled by beta adrenergic receptors and is fundamental to survival; but repeated instances of fight-or-flight over time can lead to chronic damage to the heart, contributing to heart failure development. Sathyamangla Prasad, Ph.D, who was a contributing author of the study, lent his expertise on beta-adrenergic receptors and heart failure to the investigation.A standard treatment to alleviate stress on the heart is a beta-blocker medication, which works as an on/off switch for the beta-2 adrenergic receptors. To activate the fight-or-flight pathway, hormones like adrenaline bind directly into tailor-made slots in beta 2-adrenergic receptors like a key sliding into a lock.
Beta-blockers are designed to fit into the same keyhole, preventing adrenaline and other hormones from binding to the beta-2 adrenergic receptors. This in turn causes heart rate to slow, reduces strain on the heart and opens blood vessels.
Advertisement
New Avenues for Targeted Beta-Adrenergic Receptor Regulation
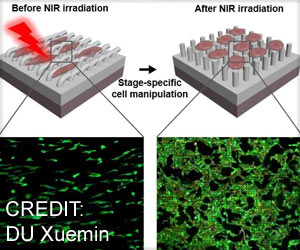
The present studies delved more deeply into determining how PAG interacts with our beta-adrenergic receptors. Prasenjit Saha, Ph.D, first author and member of Dr. Hazen’s lab, mutated different areas in the beta-2 adrenergic receptor and tested whether signaling could occur with the natural hormone epinephrine (also called adrenaline). Preclinical tests showed that mutating certain locations kept the adrenaline binding site both intact and functioning, but the mutant receptor no longer was negatively regulated by PAG.Advertisement
Dr. Hazen says his team’s findings point to an entirely new way to develop medications that regulate the beta-2 adrenergic receptor – a more nuanced regulation than what is currently on the market. They are currently working to develop drugs that target the PAG pathway and its interactions with adrenergic receptors as a new form of cardiovascular disease-treating medication.
“A beta-blocker that is more targeted in blocking the harmful signaling from the adrenergic receptors, but allowing the healthy signals through, would be an entirely new approach for treating or preventing cardiovascular disease risk,” Dr. Hazen says. “This would have the potential to improve the quality of life for patients who rely on beta-blockers to calm down their body’s stress responses”.
Reference:
- Gut microbe-generated phenylacetylglutamine is an endogenous allosteric modulator of β2-adrenergic receptors - (https://www.nature.com/articles/s41467-024-50855-3)
Source-Eurekalert