Using either patient-derived or donor-derived stem cells in heart attack, have been taken in clinical trials but thus far have not fulfilled their early promises.
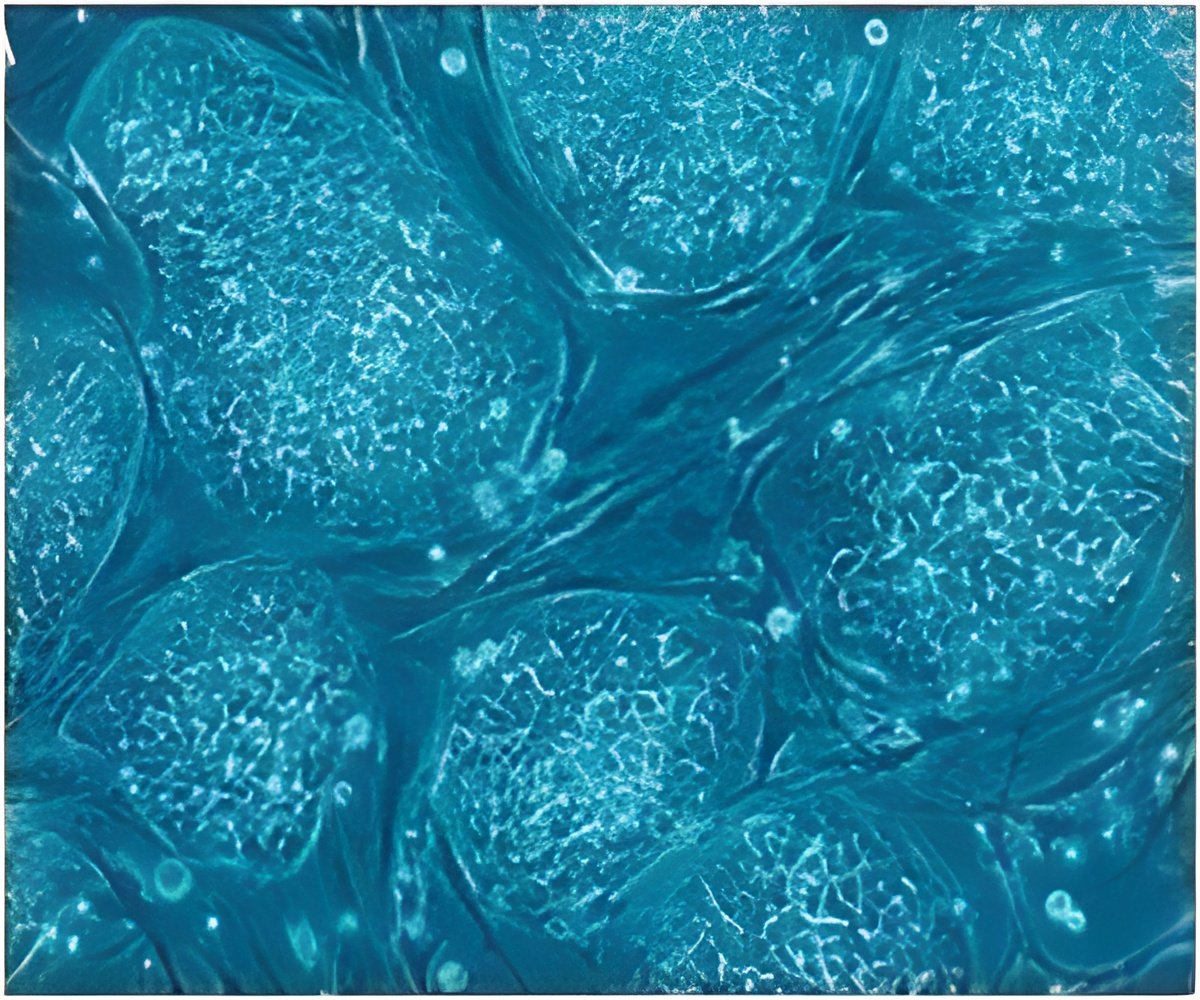
‘Stem cell-derived cardiomyocytes have weaker contractile strength than their biological counterparts isolated from heart tissue. This explain critical shortcomings of stem cell-derived heart muscle cells in clinical trials.’





A new study published in the Journal of Cell Biology by Kit Parker’s research team at the Wyss Institute for Biologically Inspired Engineering and the John A. Paulson School of Engineering and Applied Sciences (SEAS) at Harvard University suggests that stem cell-derived cardiomyocytes have weaker contractile strength than their biological counterparts isolated from heart tissue. The findings could help explain critical shortcomings of stem cell-derived heart muscle cells in clinical trials. "Our study suggests the utility of basic, in vitro cell biology studies in explaining clinical observations and pointing to potential pitfalls of cell therapies. These kinds of studies, coupled with appropriate clinical approaches, may offer a unique strategy to vet new therapeutic opportunities," said Parker, who is a Core Faculty member of the Wyss Institute and the Tarr Family Professor of Bioengineering and Applied Physics at SEAS.
To study stem cell-derived cardiomyocytes and compare their chemical and mechanical properties to those of cardiomyocytes in actual heart tissue, Parker’s team made use of a previously engineered heart muscle on-a-chip platform that supports the growth and maturation of cardiomyocytes in two-cell microtissue constructs. Pairing up stem cell-derived cardiomyocytes with each other (homogenous pairs) or with primary cardiomyocytes (heterogenous pairs) revealed surprising differences.
"We found that different types of stem cell-derived cardiomyocytes form the expected cell-cell junctions between each other and with primary cardiomyocytes. Through these junctions, cardiomyocytes aligned their contractile machineries and contracted synchronously. However, when we investigated the contractile strengths of homogeneous and heterogeneous pairs with traction force microscopy, we found stem cell-derived cardiomyocytes to be significantly weaker," said Francesco Pasqualini, who together with Yvonne Aratyn-Schaus, is a co-first author of the study.
Both performed their work as Postdoctoral Fellows in Parker’s team and Pasqualini was recently appointed a Senior Scientist at the newly founded Wyss Translational Center Zurich to continue his work in heart regenerative research. Interestingly, the team also noticed increased numbers of compensatory substrate adhesions between stronger and weaker cardiomyocytes in heterogenous pairs whose role it is to keep the pair from rupturing, but which might also transmit mechanotransductive signals.
Advertisement
In addition, the team built a computational model that can simulate the force imbalances present in heterogenous cell pairs of both murine and human stem cell-derived cardiomyocytes.
Advertisement
Source-Eurekalert