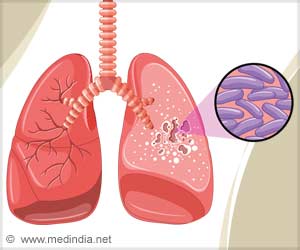
In the lungs of tuberculosis patients, the new radiotracer FDT enables PET scans to accurately identify the precise location and activity of TB.
Distributable, metabolic PET reporting of tuberculosis
Go to source). The researchers have put the new radiotracer through extensive pre-clinical trials with no adverse effects and it is now ready to go into Phase I trials in humans.
‘Not only humans can get #tuberculosis. Elephants, birds, and even seals can be infected by different strains of the bacteria. #TB’





Two methods currently exist for TB diagnosis: testing for the TB bacteria in a patient’s spit or a PET scan to look for signs of inflammation in the lung, using the common radiotracer FDG. However, a spit test can show a negative long before the disease has been fully treated in the lungs, which could result in patients finishing treatment too early.
The Limitations of Inflammation Scans in TB Detection
Scanning for inflammation can be helpful in seeing the extent of the disease, but it is not specific to TB, as inflammation can be caused by other conditions. Inflammation can also persist in the lung after the TB bacteria has been eliminated, leading to treatment continuing longer than necessary.The new approach developed by the researchers is more specific as it uses a carbohydrate that is only processed by the TB bacteria.
A key advantage of the new approach is that it only requires a hospital to have standard radiation control and PET scanners, which are becoming more widely available throughout the world. The new molecule is created from FDG using a relatively simple process involving enzymes developed by the research team. This means it can be produced without specialist expertise or laboratories and so would be a viable option in low- and middle-income countries with less developed healthcare systems. These countries currently see over 80% of global TB cases and deaths from the disease.
Advertisement
Professor Ben Davis, Science Director of the Franklin’s Next Generation Chemistry group, led the research. He said: “Finding an accurate way to identify when TB is still active in the body is not only important for initial diagnosis, but to ensure patients are receiving antibiotics long enough to kill the disease, and no longer."
Advertisement
Dr Clifton Barry III, from the National Institute of Allergy and Infectious Diseases, said: “FDT will enable us to assess in real time whether the TB bacteria remains viable in patients who are receiving treatment, rather than having to wait to see whether or not they relapse with active disease. This means FDT could add significant value to clinical trials of new drugs, transforming the way they are tested for use in the clinic.”
Reference:
- Distributable, metabolic PET reporting of tuberculosis - (https://www.nature.com/articles/s41467-024-48691-6)
Source-Eurekalert