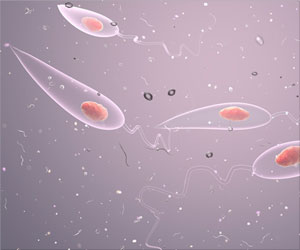
Limited evidence on drug safety and efficacy on Visceral Leishmaniasis (VL) in pregnant women is found to be associated with delayed and ineffective therapeutic choices.

‘Limited evidence on drug safety and efficacy on Visceral Leishmaniasis (VL) in pregnant women is found to be associated with delayed and ineffective therapeutic choices. However, a recent review suggests that liposomal amphotericin B (L-AmB) may be regarded as the preferred treatment for VL during pregnancy.’





“As a chronic illness, visceral leishmaniasis (VL) is usually a barrier to pregnancy or causes miscarriage early on. However, in cases where the pregnancy continues, it often results in stillbirth or the child is born with some parasites and develops VL and in the majority of cases it is fatal. The added complication of access to limited rural health facilities means that VL in pregnant women is often undiagnosed and resulting in under-reporting in regional or national health statistics and to scant literature,” says Professor Ahmed Musa, of IEND, University of Khartoum and a leading scientist on the epidemiology of VL in the East African region. Evidence on Visceral Leishmaniasis
The present review brings together scattered observations of VL in pregnant women in the clinical literature and highlights that the disease in pregnancy is under-reported and under-studied.
The findings also suggest that liposomal amphotericin B (L-AmB) is to be regarded as the preferred treatment for VL during pregnancy.
Earlier, the clinicians had to rely on personal experience or limited published case reports to make an effective therapeutic choice for VL. This led to delays in treatment and additional risks.
Advertisement
The study thereby lays the ground for better understanding of the treatment of VL in pregnancy and depicts how severe the impact of VL is on pregnant women especially in low-income settings.
Advertisement