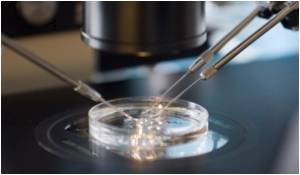
Three healthy babies have been born in a pilot study of a technique to screen eggs across the full range of chromosomes, looking for defects that boost the risk of miscarriage, doctors said Friday.
"All babies and their mothers are doing very well in terms of weight and overall developmental performance," said Cristina Magli, an embryologist at the SISMER Centre in Bologna which took part in the trial.
It is the first controlled trial of a technique called microarray comparative genomic hybridisation (CGH), which aims at boosting success in assisted reproduction.
The first birth using CGH occurred in Britain last year: a baby called Oliver, who was born to a 41-year-old woman who had had 13 failed attempts at in-vitro fertilisation (IVF).
Several other pregnancies in ESHRE's study are still under way, and plans are being set for a large-scale international clinical trial in 2011, the society said in its press release.
Human cells have 46 chromosomes, with 23 inherited from each parent. Before an egg is fertilised, it ejects half of its full set of chromosomes to make room for the 23 coming from the sperm.
Advertisement
CGH examines this cast-off genetic material. If there are too few or too many chromosomes, doctors know that the egg is not suitable for use.
Advertisement
Firstly, it tests all 23 pairs of chromosomes in a cell, rather than a limited number, as other methods do, ESHRE said.
In addition, the cell tested is taken from the egg at fertilisation, rather than from a developing embryo.
As a result, the technique could be a boon in countries which outlaw embryo analysis.
Further, by selecting an embryo that has the best chance of developing into a live birth, IVF doctors are less tempted to implant multiple embryos.
Multiple pregnancies are one of the most controversial areas of IVF, given the evidence that twins and triplets are at risk of low birth weight and developmental difficulties.
Women who would benefit most from CGH are in a category where there is higher-than-average rate of embryonic chromosomal abnormalities, ESHRE said.
These are women who are aged over 37 and have a record of unsuccessful IVF and a history of miscarriage.
"We have learnt from more than 30 years of IVF that many of the embryos we transfer have chromosome abnormalities," ESHRE's chairman, Luca Gianaroli, said.
"Indeed, it's still the case that two out of every three embryos we transfer fail to implant as a pregnancy, many of them because of these abnormalities."
The exploit reflects the widening use of DNA screening in IVF, although the principle has also hit ethical concerns -- that it could one day be abused to create "designer" babies.
Nearly four million children around the world have been born through IVF or a related technique, involving the transfer of a single sperm into the egg, since the first "test-tube" baby, Louise Brown, was born in 1978.
The scientist who pioneered the technique, Bob Edwards, won the 2010 Nobel Medicine Prize on October 4.
The Vatican lashed the award as "completely out of order," given the large numbers of embryos that are wasted. The Roman Catholic church and some evangelical conservatives contend that human life starts at the earliest state of the embryo.
Source-AFP








