The research team examined blood and bone marrow samples of 188 adults with acute myelogenous leukemia (AML) and then followed the patients' progress to gauge the…
The road to better treatment for the most common form of adult leukemia will require blocking multiple molecular pathways that fuel the disease, researchers at The University of Texas M. D. Anderson Cancer Center report in the Oct. 1 edition of the journal Blood.
The research team examined blood and bone marrow samples of 188 adults with acute myelogenous leukemia (AML) and then followed the patients' progress to gauge the cumulative impact of a trio of cell-signaling chain reactions on the disease."We found that the more of these pathways that are active in a patient, the worse their prognosis," says first author Steve Kornblau, M.D., associate professor in the Department of Blood and Marrow Transplantation.
Patients who had none of the three molecular cascades active had a median survival time of 78.6 weeks. For those with one highly active pathway, median survival was 57.9 weeks. With two, it was 42.3 weeks. Patients with high activation of all three pathways had a median survival time of just 23.4 weeks.
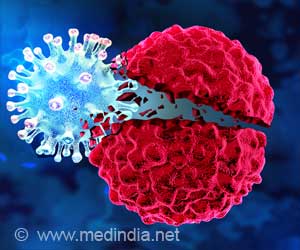
"Targeting just one of these pathways won't be effective because we also found that they cross-activate each other, they essentially cover for each other," Kornblau said. "New therapies will have to target multiple pathways to be effective."
This presents several challenges to discovering a successful treatment for AML, the research team noted. New drugs are typically evaluated individually during development, so a medication that blocks one of these pathways is likely to fail to treat AML by itself. It would probably be discarded as a single therapy when it could become part of a multiple-drug attack on the disease.
Finding a multi-drug therapy also will require an unprecedented degree of cooperation among pharmaceutical firms and academic investigators holding the rights to different agents that are active in different molecular pathways, Kornblau and colleagues noted.
Advertisement
"This compensatory ability suggests that the use of single "targeted" agents may be suboptimal, a concept that, unfortunately is all too well supported by clinical experience in all malignancies and has broad implications for the entire field of cancer therapeutics," writes Judith Karp, M.D., of the Sidney Kimmel Cancer Center at Johns Hopkins.
Advertisement
AML occurs when abnormal blood cells rapidly build up in the bone marrow, interfering with the production of normal blood cells. While chemotherapy often places the disease in remission, it usually comes back. Only about 20 percent of patients are cured with chemotherapy, and another 10 percent are successfully treated with bone marrow transplants.
One of the great successes of cancer treatment has been development of targeted therapy for chronic myelogenous leukemia (CML). The drug Gleevec and its successors inhibit one aberrant protein, increasing the median 5-year survival of CML patients from 50 percent to 90 percent. For AML, that approach won't work. "AML is more complicated, with multiple means of activation," Kornblau says.
The research team looked at activation of three components, one from each pathway, in the leukemic blasts found in newly diagnosed patients. Activation of each component - PKCa, pERK2 and pAKT - had an adverse effect on the patient's prospects that was independent of other traditional prognostic factors. Their cumulative impact was greater than simply adding their individual effects would suggest, the research team found.
Source-Newswise
SRM