Thyroid cancer survivors reported an average of 5.56 out of 10 on the scale for mean quality of life, which was worse than the score reported by survivors of other cancer.
‘Thyroid cancer is the 8th most-common cancer in the U.S., with about 62,000 new cases diagnosed this year, according to National Cancer Institute data.’





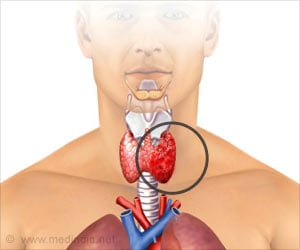
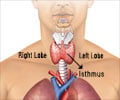
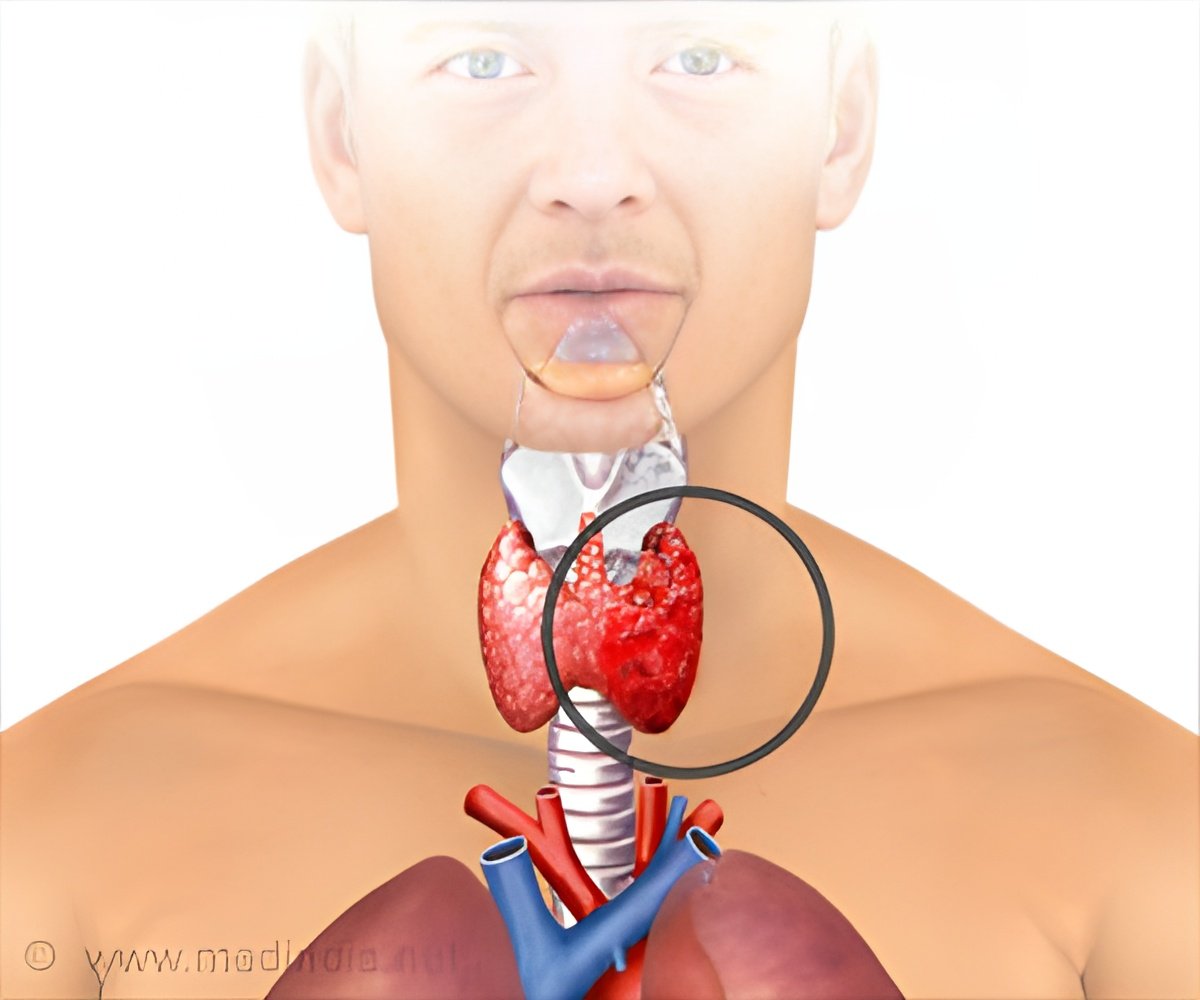
Thyroid cancer patients have a nearly 98 percent five-year survival rate, according to the National Cancer Institute. More than 95 percent survive a decade, leading some to call it a "good cancer." But those successful outcomes mean few thyroid cancer survivorship studies have been conducted. UChicago Medicine researchers Briseis Aschebrook-Kilfoy, PhD, assistant research professor in epidemiology, and Raymon Grogan, MD, assistant professor of surgery, are trying to address that data gap. Together, they lead the North American Thyroid Cancer Survivorship Study (NATCSS).
For their most recent research, Aschebrook-Kilfoy and Grogan recruited 1,174 thyroid cancer survivors - 89.9 percent female with an average age of 48 - from across the U.S. and Canada. Participants were recruited through the thyroid cancer clinics at UChicago Chicago Medicine, the clinics of six other universities, as well as through thyroid cancer survivor support groups and social media.
The researchers then used City of Hope's Quality of Life thyroid tool, a questionnaire that assesses physical, psychological, social and spiritual wellbeing to measure patient-reported quality of life. They found that thyroid cancer survivors reported an average of 5.56 out of 10 on the scale. That was worse than the mean quality of life score of 6.75 that was reported by survivors of other cancer types (including colorectal and breast cancer) that have poorer prognoses and more invasive treatments.
"I think we all have this fear of cancer that has been engrained in our society," Grogan said. "So, no matter what the prognosis is, we're just terrified that we have a cancer. I think this shows that."
Advertisement
Aschebrook-Kilfoy and Grogan also found that patients who were younger, female, and less educated, as well as those who participated in survivorship groups, all reported even worse quality of life than other study participants. However, after the five-year mark, quality of life gradually starts to increase over time for both male and female thyroid cancer survivors.
Advertisement
"The goal of this study is to turn it into a long-term, longitudinal cohort," said Grogan, who hopes to develop a tool that physicians can use to assess the psychological wellbeing of thyroid cancer survivors. "But, there was no way to do that with thyroid cancer because no one had ever studied quality of life or psychology of thyroid cancer before."
Psychological wellbeing is part of the Institute of Medicine's recommended survivorship care plans.
Thyroid cancer rates have increased dramatically in the past several decades, climbing about 5 percent a year. A 2011 study by Aschebrook-Kilfoy and Grogan found that thyroid cancer, which is most common in women, will double in incidence by 2019.
"The increase that we've seen in the U.S. we've also seen in a number of countries worldwide," Aschebrook-Kilfoy said. "And, even in lower incidence countries, you see a similar gender disparity."
Both researchers believe the rise in thyroid cancer rates could be due in part to more advanced imaging tools that catch cases that might have otherwise gone undiagnosed. They also attribute it to emerging environmental and lifestyle risk factors.
"Radiation exposure is one of the main risk factors that is known to cause cancer of the thyroid," Grogan said. "One environmental hypothesis is that ultra-low doses of radiation over decades could cause some type of change in the thyroid."
Another common environmental hypothesis: pesticides and other chemicals in the environment have been shown to affect thyroid hormone levels, an area where Aschebrook-Kilfoy has focused much of her research.
"Along with that there is literature that shows there's an increased risk of thyroid cancer with people who are obese," she said.
Other studies have even shown that proximity to volcanic activity (living in a certain region on the Italian island of Sicily, for example) correlates with an increased risk for the disease. Scientists are still not sure why.
Aschebrook-Kilfoy and Grogan have begun to collect biospecimens and DNA samples from patients, which can be used to further study environmental and genetic risk factors that may account for the increase.
Both researchers hope this study will demonstrate the importance of studying survivorship, especially in thyroid cancer, which may have better patient outcomes but is far from "good."
Source-Eurekalert