Hip replacement surgeries may not only improve the quality of life but also increase life expectancy in elderly, finds a new study.
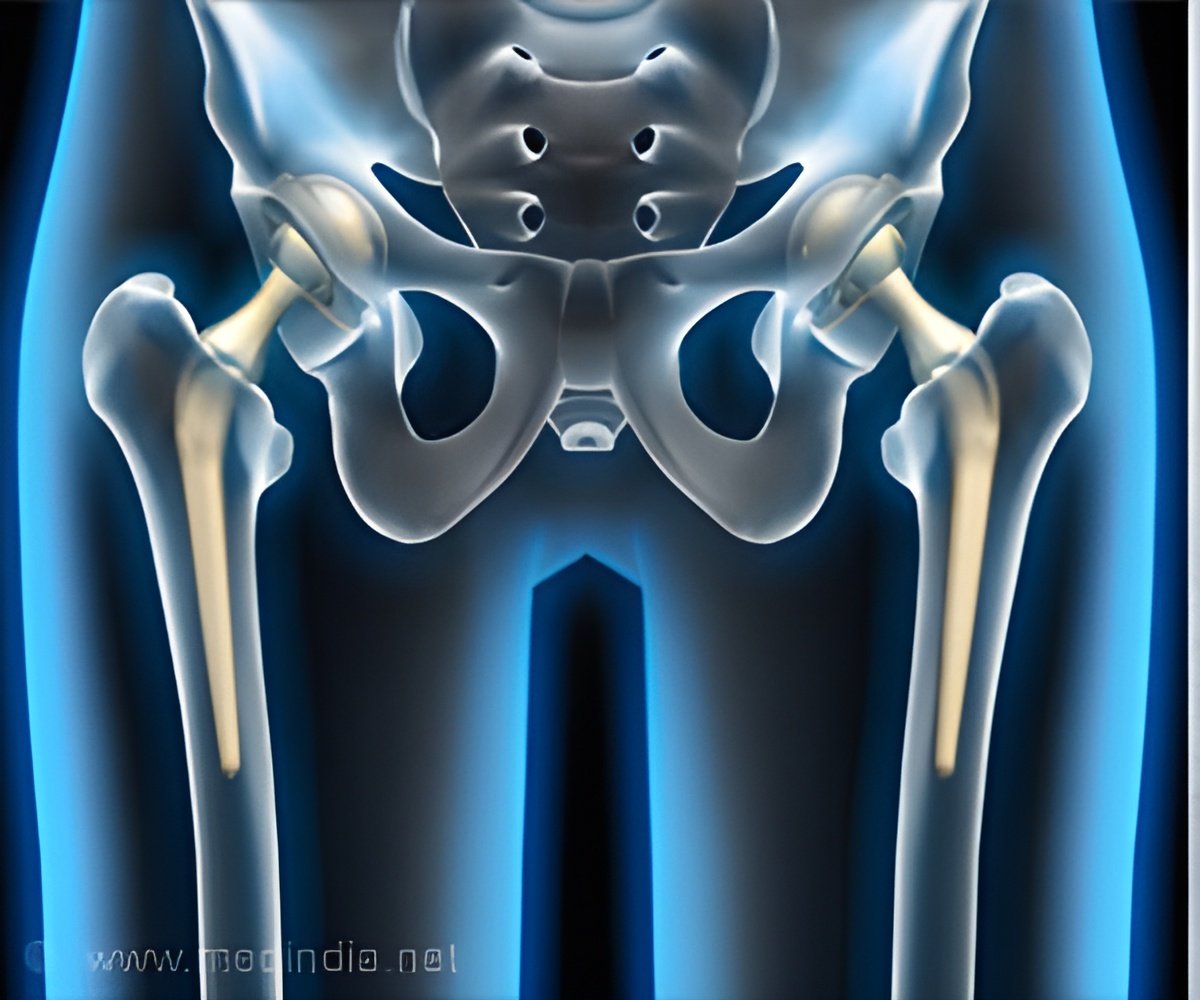
‘Survival of elderly patients after a total hip replacement has seen significant improvement, and that patients undergoing THA tend to live longer than a matched general population. The surgery has a proven track record of increasing mobility, reducing pain, and improving quality of life in people with hip pain and dysfunction.’





Through Ten Years, Higher Survival in Patients Undergoing Hip Arthroplasty. The researchers analyzed postoperative survival rate in nearly 132,000 patients undergoing THA in Sweden from 1999 through 2012. Average age at hip replacement was about 68 years. During a median follow-up of 5.6 years, about 16.5 percent of patients died.Survival after THA was longer than expected, compared to people of similar age and sex in the general Swedish population. In the first year, survival was one percent better in THA patients versus the matched population.
The difference increased to three percent at five years, then decreased to two percent at 10 years. By 12 years, survival was no longer different for THA patients compared to the general population.
The survival difference was significant mainly among patients diagnosed with primary osteoarthritis. This condition, reflecting age-related "wear and tear," accounted for 91 percent of patients undergoing THA. In patients with certain other diagnoses--including osteonecrosis, inflammatory arthritis, and "secondary" osteoarthritis due to other health conditions or risk factors--survival after THA was lower compared to the general population.
Not surprisingly, patients with more accompanying medical conditions (comorbidity) had lower survival after THA. Lower education and single marital status were also associated with lower survival.
Advertisement
"The reasons for the increase in relative survival are unknown but are probably multifactorial," the researchers write. They note some important limitations of their registry study, including the fact that that only patients in relatively good health are selected for THA.
The study provides new insights into the lifelong health benefits and economic value of THA, according to an accompanying CORR Insights® article by Hannes A. Rüdiger, MD, of Schulthess Clinic, Zurich. Especially as the procedure is performed in younger patients, information on the long-term rates of repeat (revision) surgery will be essential. Dr. Rüdiger writes, "As surgeons, we need more data in order to advise a patient about what one can and cannot expect from intervention and how it will affect them for the rest of their lives."
Source-Eurekalert