Rapamycin-a transplant anti-rejection drug actually demonstrated benefits in a mouse having a fatal defect in the mitochondria
Reporting this week in Science Express, University of Washington researchers said that they found that treatment with rapamycin "robustly enhances survival and attenuates disease progression in a mouse model of Leigh's syndrome." Given as a daily injection, the drug delayed the onset of neurological symptoms, reduced brain inflammation, and prevented brain lesions.
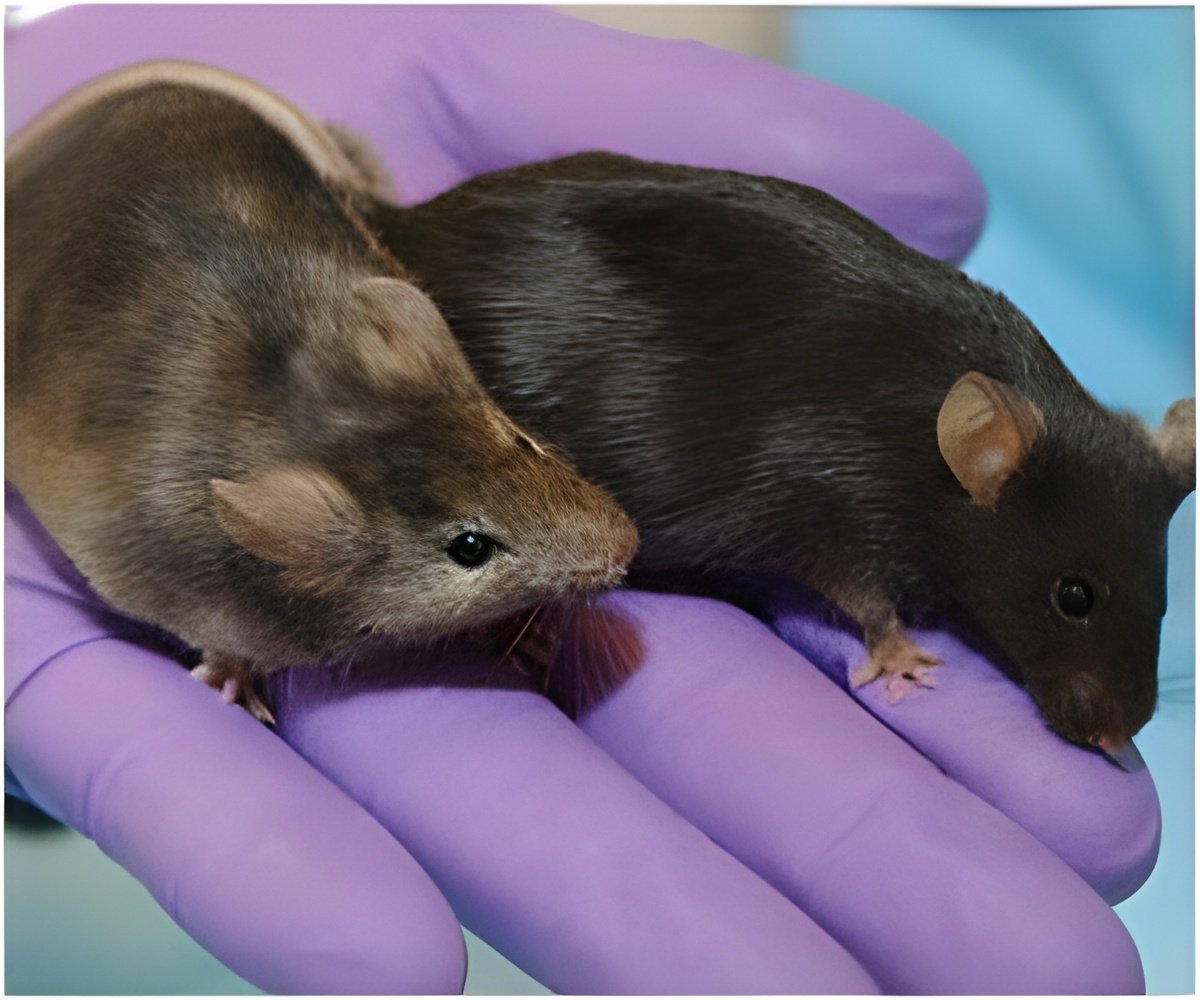
For most of their lives, the treated mice breathed normally, and did not clasp their legs against their bodies, a posture characteristic of this and related brain disorders in mice. Unlike the untreated mice, they could balance and run on a rotarod, a miniature log rolling exercise toy. Both the median and maximum lifespans within the group of treated mice were strikingly extended, the authors noted.
The median lifespan for this mouse condition is 50 days. In comparison, treated males lived a median of 114 days, and females 111 days. The longest survival in the treated group was 269 days, more than triple that of the untreated animals.
"We were excited at the findings because of the potential impact on treatment for kids with this or related mitochondrial diseases," said the senior author of the study, Dr. Matt Kaeberlein, associate professor of pathology at the University of Washington. "Similar intervention strategies might also prove useful for a broad range of mitochondrial diseases or for other conditions resulting from mitochondrial dysfunction."
Mitochondrial defects lessen the amount of energy available to cells. The depletion can damage or destroy vital tissues. Symptoms and severity of illness depends on which types of cells are affected, but in many cases several organ systems operate poorly as a consequence of malfunctioning mitochondria.
Advertisement
Kaeberlein, whose research focus has been factors that lengthen life, has been studying the anti-aging effects of rapamycin for several years. The drug, like calorie-restricting diets, acts by inhibiting mTOR, an abbreviation for the eponymously named mechanistic target of rapamycin.
Advertisement
Alongside their work in aging and lifespan in normal mice, Kaeberlein and his lab decided to study rapamycin's actions on mice with a severe mitochondrial defect. The mouse model for Leigh syndrome was created in the University of Washington laboratory of Dr. Richard Palmiter, a professor of biochemistry and Howard Hughes Medical Institute investigator who was one of the early originators of transgenic mouse models. The research team included Dr. Philip G. Morgan and Dr. Margaret M. Sedensky, from the Department of Anesthesiology and Pain Medicine at Seattle Children's Hospital, who study mitochondrial diseases in patients. The lead scientist was Simon C. Johnson from the UW Department of Pathology.
After seeing the unexpected benefits on health and survival, the research group looked more closely at the effects on metabolism by examining the levels of more than 100 different metabolites – cellular building blocks and intermediates used to make energy – in the treated and untreated Leigh syndrome mice. The team observed that the treated mice appear to be burning more amino acids and fats as an energy source, rather than the sugar, glucose. This eliminated the accumulation of glucose breakdown byproducts, including lactate. These byproducts can be toxic and are seen at high levels in human Leigh syndrome patients.
"The drug did not substantially alter mitochondrial composition. Instead, the mice appear to be bypassing the deficiency in their mitochondria through a shift in their metabolic pattern," Kaeberlein said. "However, we can't yet explain exactly how this rescues the mice with Leigh syndrome."
Because this was a mouse study, evidence ofefficacy of rapamycin in Leigh syndrome patients will be a necessary next step. Rapamycin already has FDA approval for several uses, including preventing organ transplant rejection and for treating rare forms of cancer; however, the drug also has side-effects which might limit its utility in very young children. Kaeberlein is optimistic, however, that "even if rapamycin doesn't turn out to be be useful as a treatment for Leigh Syndrome, the lessons learned here will pave the way to new therapies for this devastating disease."
Source-Eurekalert









