An approach proven to cure a rat model of type 1 or juvenile-onset diabetes also works in a rat model of type 2 or adult-onset diabetes.
An approach proven to cure a rat model of type 1 or juvenile-onset diabetes also works in a rat model of type 2 or adult-onset diabetes, according to a new report from researchers at Washington University School of Medicine in St. Louis.
"Finding that we can cure type 2 diabetes in the same way is very significant because in humans type 2 diabetes is almost 20 times more prevalent than type 1 diabetes," says senior author Marc R. Hammerman, M.D., the Chromalloy Professor of Renal Diseases in Medicine. "There are about 200 million type 2 diabetics worldwide, and the incidence is rapidly increasing."The treatment approach transplants precursors of the pancreas from embryonic pigs. In a previous study, Hammerman and co-developer Sharon A. Rogers, research instructor in medicine, showed that they could transplant the cells in a way that lets them grow into insulin producers without triggering attacks by the rats’ immune systems. This cured the rats' diabetes without the risky immune suppression drugs required to prevent rejection in other transplant-based treatments.
Hammerman and Rogers are leaders in the emerging field of organogenesis, which focuses on growing organs from stem cells and other embryonic cell clusters known as organ primordia. Unlike embryonic stem cells, which can become virtually any cell type, primordia are locked into becoming cells of a particular organ.
Their approach for diabetes treatment uses pig pancreatic primordia. In previous research, they found that obtaining the primordia early in the pigs' development rendered them "invisible" to the rats' immune system, eliminating the need for antirejection drugs.
In the new study, they transplanted the pig primordia into a strain of rat with a disorder that closely resembles human type 2 diabetes. The result was the same: the transplants cured the rats’ diabetes without any immune suppression.
Hammerman notes that the new study shows the lack of immune rejection wasn't just an artifact from the strain of rats used for the first experiments.
Advertisement
One distinction between the two types of diabetes that made such a prediction difficult is the phenomenon known as insulin resistance. Levels of blood sugar are high in type 1 diabetics because insulin-producing pancreas cells have been destroyed. In contrast, blood sugar is high in type 2 diabetics in part because tissues become insensitive or resistant to insulin. The pancreas becomes irreparably damaged in an effort to keep up with the resulting increase in insulin demand.
Advertisement
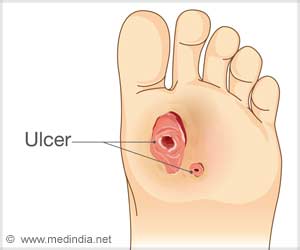
As a diabetes treatment for human patients, pig insulin works as well as the human form. However, administering either type of insulin via injection does not control blood sugar well enough to prevent diabetic complications.
In contrast, insulin-producing cells in transplants secrete insulin only in response to elevated blood sugar levels, stopping when glucose levels are normal.
Hammerman and Rogers showed that engrafted embryonic pig pancreatic tissue removed from rats and placed in a test tube releases pig insulin within a minute of being exposed to high glucose levels.
"The link between the glucose-sensing and insulin-releasing machinery of the pig cells is established normally after transplantation of primordia, and they work just like a normal pancreas,” says Rogers.
The advantages of transplanting insulin-producing cells has also led to decades of research into transplantation of human pancreas and islets, the cells that produce insulin. Unfortunately, donor organs are so scarce that transplantation is an option for only a tenth of 1 percent of type 1 diabetics. Such transplants are almost never performed to treat type 2 diabetes.
"Furthermore, transplant recipients require antirejection drugs, so they are trading one disease, diabetes, for another, immune suppression," says Hammerman. "If pig pancreatic primordia prove to be comparably invisible to the human immune system, they could represent a virtually unlimited source of donor organs to treat human diabetes without the need for host immune suppression.”
Source-Newswise
SRM