Estimates from the American College of Rheumatology (ACR) reveal that there are nearly 300,000 children with juvenile arthritis and other rheumatic illnesses in the U.S.
Estimates from the American College of Rheumatology (ACR) reveal that there are nearly 300,000 children with juvenile arthritis and other rheumatic illnesses in the U.S. For pediatric patients with systemic juvenile idiopathic arthritis (JIA), effective treatment for this disabling disease is imperative. New treatment recommendations that guide physicians caring for children with systemic JIA are now published in the ACR journals,
Arthritis & Rheumatism and
Arthritis Care & Research.
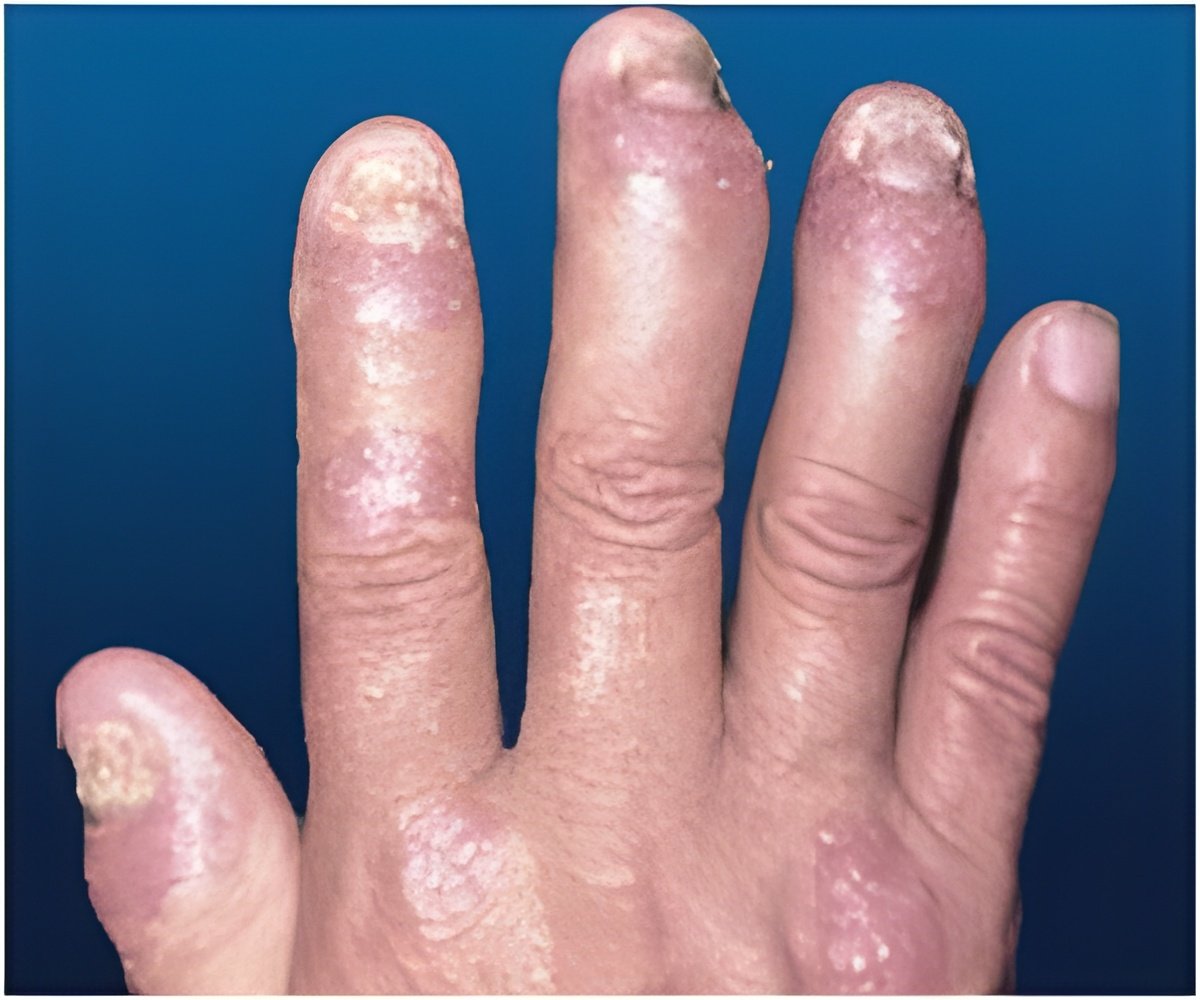
Systemic JIA is defined by the International League of Associations for Rheumatology as arthritis in one or more joints for at least six weeks in children sixteen years of age or younger. The arthritis is accompanied or preceded by fever for at least two-weeks that is daily ("quotidian") for at least 3 of those days, with one or more of the following symptoms: red rash (evanescent erythematous rash), enlarged liver, spleen or lymph nodes, and inflammation of the tissue lining (serositis) of the lungs, heart, or stomach. Medical evidence suggests that systemic JIA accounts for 4% to 15% of all JIA cases.
Each year the ACR reviews its current guidelines to ensure that they are up to date. In 2012, the ACR determined that an update to the 2011 JIA recommendations—specifically for treatment of systemic JIA—was needed. A new team that included researchers who worked on the original JIA guideline was assembled to develop the 2013 update. Investigators, led by Dr. Pamela Weiss from Children's Hospital of Philadelphia in Pennsylvania and Dr. Sarah Ringold from the Seattle Children's Hospital in Washington, conducted a systematic review of medical literature through January 2013.
The new recommendations for systemic JIA are based upon more than 1,200 clinical scenarios and include recommendations for use of the following medications:
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Glucocorticoids
- Methotrexate
- Leflunomide
- Intravenous immunoglobulin (IVIG)
- Calcineurin inhibitors
- Tumor necrosis factor alpha (TNFα) inhibitors
- Abatacept
- Rituximab
- Anakinra
- Canakinumab *
- Rilonacept *
- Tocilizumab *
*New addition to the 2013 update
They include treatment options for patients with and without active systemic disease, along with varying degrees of inflammation of the joint lining (synovitis), as well as recommendations for repeat TB screening for JIA patients receiving biologics. Dr. Weiss concludes, "The 2013 recommendations address specific disease characteristics and reflect the commitment to enhancing care of children with systemic JIA."
Source-Eurekalert