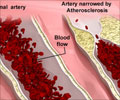
Medicare beneficiaries in some parts of the United States appear more likely to receive carotid endarterectomy, a surgical procedure to clear blockages in the artery supplying blood

A 2004 national coverage decision supported the use of carotid artery stents for Medicare beneficiaries with symptomatic disease and at high risk for surgery or participating in a clinical trial. To identify patterns in the use of stents or endarterectomy since this decision, Manesh R. Patel, M.D., of Duke University School of Medicine, Durham, N.C., and colleagues analyzed claims of patients age 65 and older from the Centers for Medicare & Medicaid Services from Jan. 1, 2003, through Dec. 31, 2006.
During this time period, nationwide rates of carotid endarterectomy among Medicare beneficiaries decreased from 3.2 per 1,000 patients per year to 2.6 per 1,000 patients per year. The claims codes for stenting first appeared in the data in 2005; 0.3 procedures were performed per 1,000 patients that year, and 0.4 per 1,000 patients received stents in 2006.
After adjusting for demographic and clinical characteristics, a significant geographic variation was found in the odds of revascularization. The New England, Mountain (Arizona, Colorado, Idaho, Montana, Nevada, New Mexico, Utah and Wyoming) and Pacific (Alaska, California, Hawaii, Oregon and Washington) regions tended to have the lowest rates of both procedures, whereas the East South Central (Alabama, Kentucky, Mississippi and Tennessee), East North Central (Illinois, Indiana, Michigan, Ohio and Wisconsin) and West North Central (Iowa, Kansas, Minnesota, Missouri, Nebraska, North Dakota and South Dakota) regions had the highest rates. There was nearly a nine-fold difference between the highest and lowest rate of endarterectomy across regions in 2003 and 2004 and a seven-fold difference in 2005 and 2006.
In 2005, 1.2 percent of patients had died 30 days after endarterectomy and 6.8 percent had died after one year. This compares with death rates of 2.3 percent after 30 days and 10.3 percent after one year for carotid stenting.
"Significant geographic variation was seen in the use of carotid endarterectomy and carotid stenting among Medicare beneficiaries and variation in the carotid imaging modalities used before revascularization," the authors write. "Moreover, men and patients with a prior diagnosis of peripheral vascular disease were more likely to undergo carotid revascularization, and patients with a prior diagnosis of coronary artery disease or a prior carotid endarterectomy were more likely to undergo carotid stenting. These findings suggest that the development of consensus regarding clinical criteria for carotid imaging, such as a national standard for appropriate use criteria, is required."
Advertisement