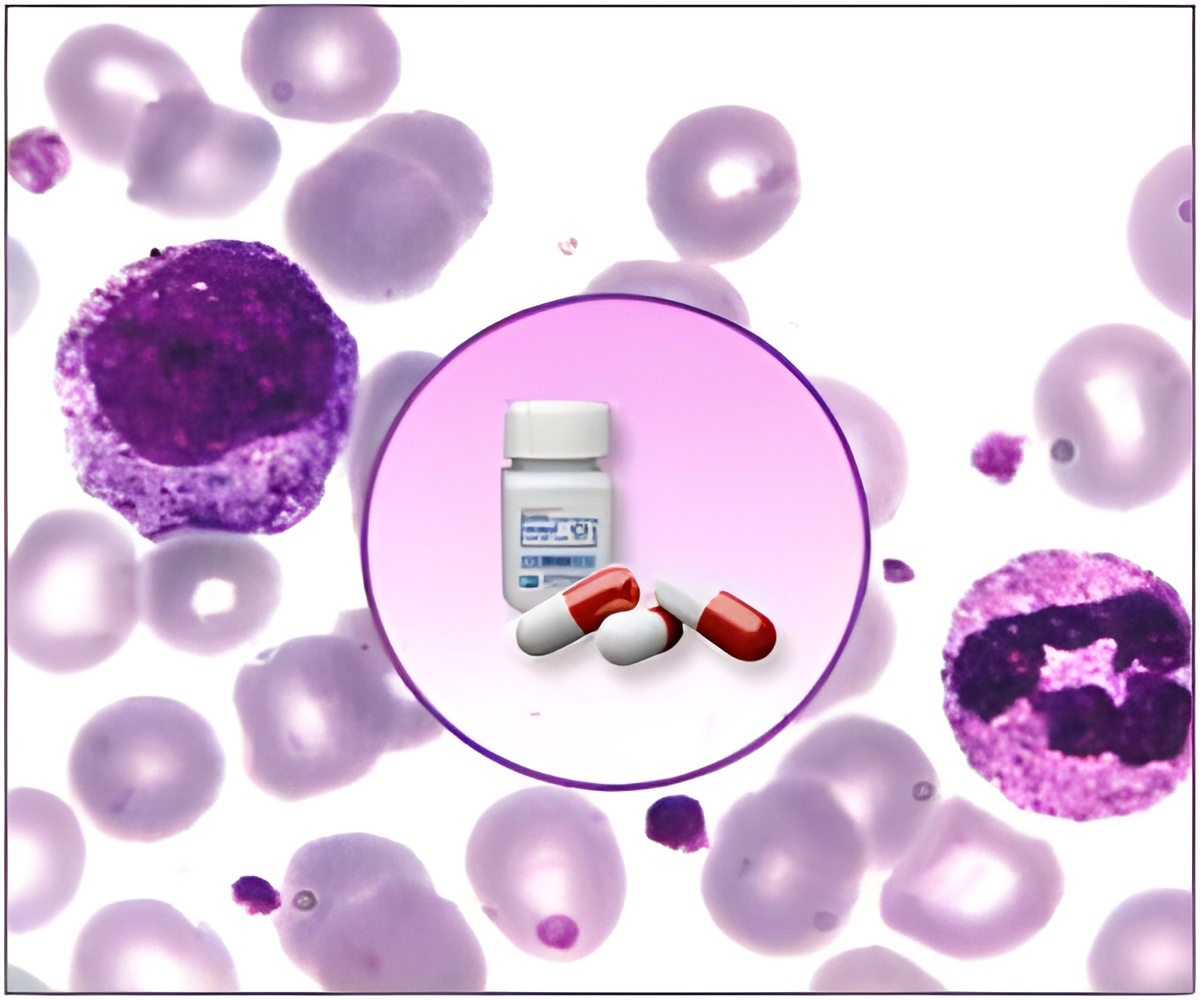
A new study reveals that providing a weekly or a monthly dose of a combination of a potent chemotherapy drug with a monoclonal antibody can help it selectively target malignant cells.
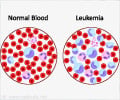
"The CD22 antigen is a specific marker for B-cell malignancies and is expressed in more than 90 percent of patients who have acute lymphocytic leukemia," said Susan O'Brien, M.D., professor in The University of Texas MD Anderson Department of Leukemia. "The antigen's specificity for B-cell cancers makes it a promising therapeutic target for intervention."
Bound to a potent toxin The humanized antibody, known as inotuzumab ozogamicin, is attached to the toxin calicheamicin and binds to CD22. "After binding to the B cell, the antibody is internalized and the linker hydrolyzed, releasing the calicheamicin into only the malignant B cell," O'Brien said. "This enables us to bring in a very potent toxin that could not be given systemically and direct that toxin to the malignant B cell."
The experimental drug was first used in patients with B cell lymphoma. The main toxicity seen in the lymphoma trials was myelosuppression due primarily to deficiency of platelets.
"Myelosuppression is much less of an issue with acute leukemia, whether ALL or acute myelogenous leukemia, because you want to transiently wipe out the bone marrow to eradicate the leukemic cells," O'Brien said. "You expect to have myelosuppression as part of the therapy."
Toxicities manageable For this study, the researchers used the dose defined as tolerable in the lymphoma trials-1.8 mg/m2-as a starting point.
Advertisement
Amended protocol The researchers amended their protocol in an attempt to minimize toxicities. "We wondered whether we could reduce infusion reactions and liver function test elevations by giving the agent on a weekly basis instead of as a bolus every three to four weeks," O'Brien said. "The maximal plasma levels potentially would be lower, but the area under the curve might be the same because we would be giving the same total dose, just spread over three weeks."
Advertisement
The Take-Away "We observed impressive activity in a relapsed, refractory population," O'Brien said. "The toxicities were acceptable and were mainly grade 1-2 reactions to the drug itself, which is not uncommon because most antibodies are associated with mild infusion reactions. Transaminase elevations were predominately grade 1-2, and in the trial as a whole, fewer than five percent of the patients experienced grade 3-4 liver elevations."
O'Brien added that a new trial at MD Anderson is incorporating the antibody with low-dose chemotherapy as a frontline regimen for ALL in patients over age 65.
"One of the biggest complications in treating older patients with ALL is that the treatments cause myelosuppression, which makes patients more vulnerable to infection, and older patients are particularly susceptible to this and other complications," she said. "The idea is to take a very well-tolerated antibody and combine it with chemotherapy. That way we might not have to use full-dose chemo and can reduce side effects."
Source-Eurekalert