Two new risk indicators for prostate cancer will be unveiled at the 2011 European Multidisciplinary Cancer Congress today.
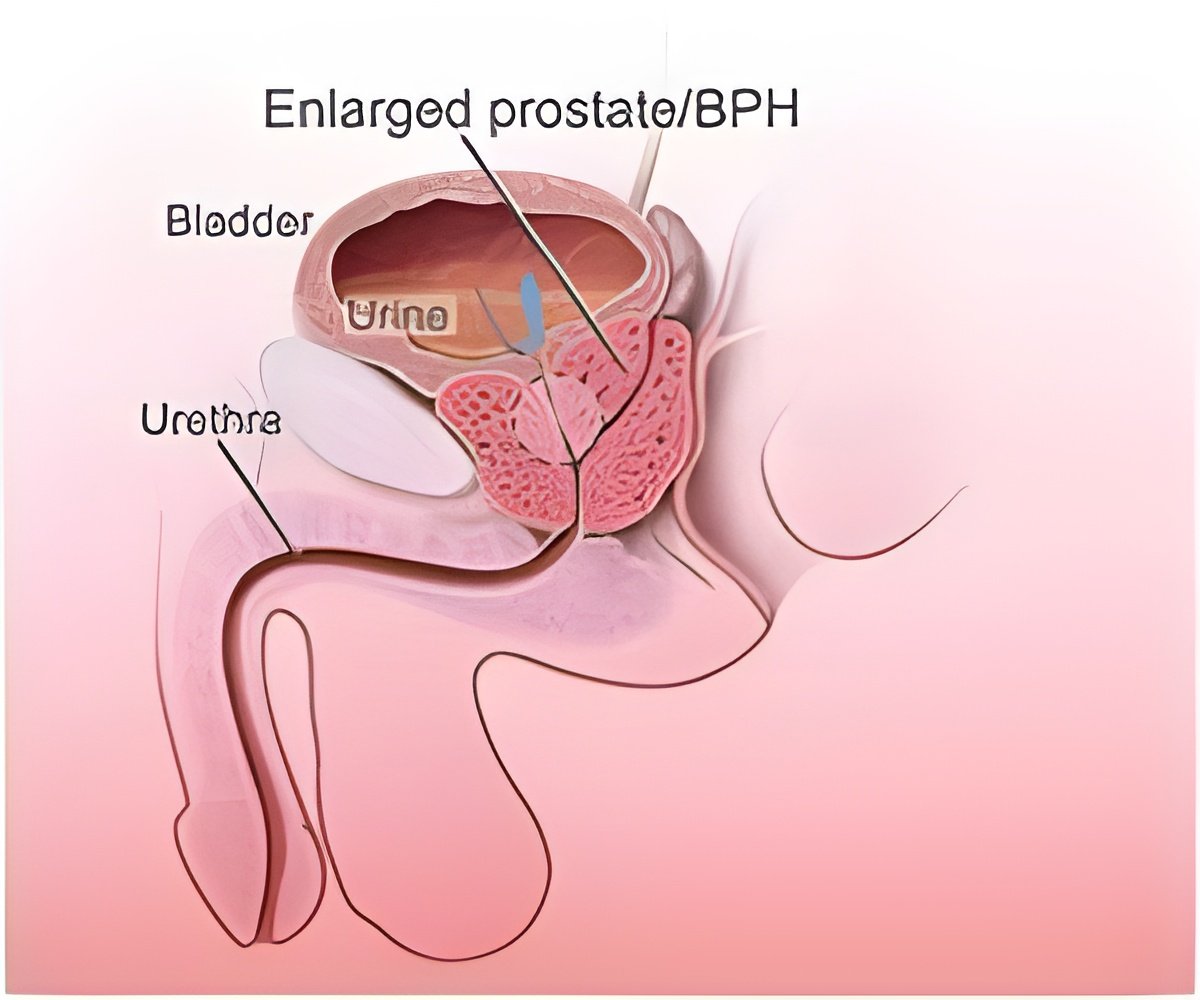
According to European Cancer Observatory statistics, over 70,000 men die from prostate cancer in the EU every year. Prostate cancer and benign enlargement of the prostate gland, known as benign prostatic hyperplasia, share common features. Growth of the gland is dependent on hormone levels in both conditions and both respond to anti-androgen treatment, but until now benign prostatic hyperplasia has not been considered a precursor to the development of a tumour.
Researchers investigated the association between the two conditions by examining data from five national registries, on a total of 3,009,258 Danish men.
The sample included 53,315 diagnoses of prostate cancer and 25,459 cases of death due to prostate cancer. Clinical benign prostatic hyperplasia was determined by records of hospitalisation (187,591 men) and/or operations for the condition (77,698 men) between 1980 and 2006, and the use of certain drugs indicated for the condition between 1995 and 2006 (143,365 men and 47,465 men respectively for the two treatments). The reference group was men without benign prostate hyperplasia.
Over 27 years, the study found that clinical benign prostate hyperplasia was associated with a two to three-fold increased risk of men developing prostate cancer, and with a two to eight-fold increased risk of them dying from prostate cancer.
"Benign prostatic hyperplasia and prostate cancer are the most common prostatic conditions with a large number of incident and prevalent cases each year. A possible association has been debated for several years but previous studies have generated ambiguous results. Our study is the largest to date and has consistent results showing an association," research team member Dr Stig Bojesen will tell the congress.
Advertisement
The second Danish study, also led by Dr Ørsted, looked at whether prostate-specific antigen levels could predict prostate cancer incidence and mortality in the general population.
Advertisement
Researchers looked at blood collected from 4,383 men aged between 20 and 94 years of age from the general population, who had taken part in the Copenhagen City Heart Study and followed them from 1981 through to 2009. They measured baseline levels of prostate specific antigen and investigated whether this correlated with later prostate cancer incidence and mortality.
During the 28 years of follow-up covered by the Heart Study, 170 men in the sample developed prostate cancer and 94 died from the disease. Measuring the antigen levels, the researchers found that stepwise increases in prostate-specific antigen predicted a 3-44 fold increased risk of prostate cancer and a 2-12 fold increased risk of prostate cancer mortality.
They also found that the absolute 10-year risk of prostate cancer was 11-22% in those with prostate-specific antigen levels of 4.01-10.00 ng/ml and 37-79% in those with levels above 10.00 ng/ml.
The ranges are wide and the higher risk for some men can be explained, Dr Ørsted will tell the congress. "The high risk for some men is probably due to some of the participants having already developed sub-clinical prostate cancer at the time of their entry to the study. These men would have had a shorter time from study entry to diagnosis and consequently, higher risk estimates."
The results could be used to target specific sections of the population for screening. "One of the major problems in prostate cancer is over-diagnosis. Furthermore, two large randomised studies have shown that the benefit of general screening for prostate cancer is limited," explains Dr Ørsted. "Our results indicate that physicians could focus screening efforts on men with higher baseline prostate specific antigen values while men with lower levels could avoid having frequent and unnecessary diagnostic examinations. This could reduce over-diagnosis and unnecessary treatment as well as reduce expenditure in already strained health systems," he says.
President of ECCO, Professor Michael Baumann, said: "These studies demonstrate how important it is to have good cancer registries and skilled cancer epidemiologists available. Large cancer registries, which contain high quality data and link to several items, enable us to address specific questions; for example, whether there is a link between benign prostate hyperplasia or long-term PSA levels and the risk of prostate cancer. Such research allows us to draft hypotheses for further research and to create more efficient screening and prevention programmes."
ESMO spokesperson, Professor Hein Van Poppel, Director of the European School of Urology, commented: "The first study indicates the need for future research to focus on how to follow patients with benign prostatic hyperplasia in order to recognise an eventual cancer in time. PCA3, genetic fusion markers or methylation markers could be explored for this purpose.
"For PSA screening, the ideal screening timetable needs to be investigated. It could well be that screening needs to start at an age where there is no interference from benign prostatic hyperplasia in PSA production, i.e. at age 40; by repeating the PSA measurement at 45 and at 50 years old, the PSA slope can probably recognise those with a high likelihood of ever developing cancer, but also those who will not need further screening because their chance of ever developing significant prostate cancer is minimal."
Source-Eurekalert


![Prostate Specific Antigen [PSA] & Prostate Cancer Diagnosis Prostate Specific Antigen [PSA] & Prostate Cancer Diagnosis](https://images.medindia.net/patientinfo/120_100/prostate-specific-antigen.jpg)










