Similar rates of success and safety found in two surgical treatments for a form of pelvic hernia affecting women, say scientists.
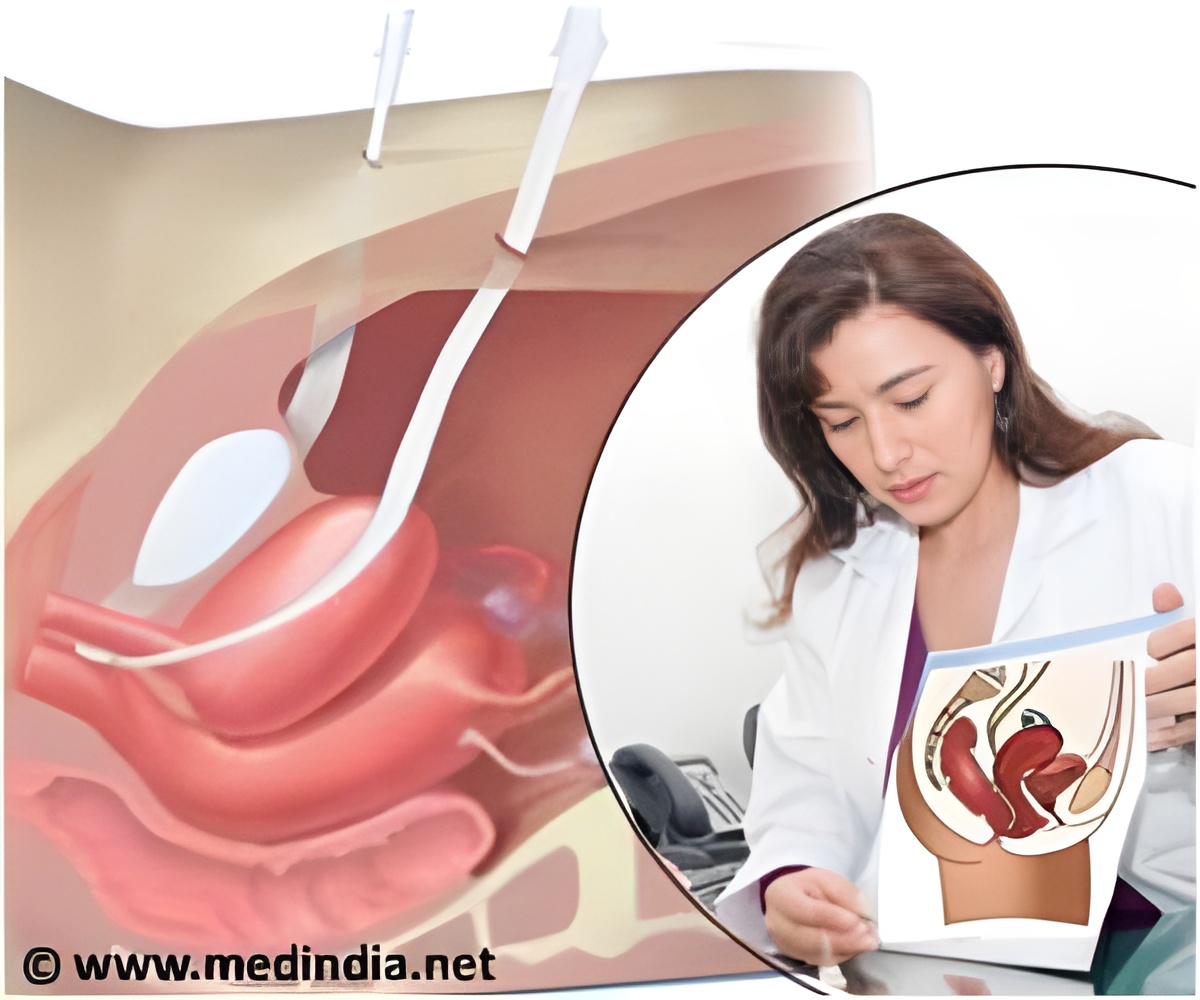
Normally, a sling of muscle and tissue spans the bottom of the pelvic cavity, holding the bladder, uterus, and other organs in place. In pelvic organ prolapse, this sling weakens, and the internal organs slump downward, pressing on the vagina and anus. In some cases, the pressure causes the vagina to invert and protrude through the vaginal opening. Symptoms may also include urinary or fecal incontinence and pelvic pain.
According to the study authors, every year, about 300,000 U.S. women undergo surgery for prolapse. In two of the most common surgeries for the condition, surgeons stitch the top of the vagina to ligaments inside the pelvic cavity. One procedure, uterosacral ligament suspension, involves stitching the vagina to the uterosacral ligaments, which normally connect the lower part of the womb to the tailbone. The other procedure, sacrospinous ligament fixation, involves stitching the top of the vagina to one of two sacrospinous ligaments, which link the lower tailbone to the pelvis.
Many women who undergo surgery for pelvic organ prolapse also receive one-on-one sessions with a specialized physical therapist or nurse who coaches them on exercises for the pelvic floor. Similar to Kegels, these exercises are meant to strengthen the pelvic floor muscles.
"This is the largest, most comprehensive study of its kind to compare these two surgical procedures and examine the potential for added benefit from pelvic floor muscle training," said study author Susan Meikle, M.D., project scientist for the Pelvic Floor Disorders Network of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). "The results provide sound information that patients and their physicians can use to plan the most appropriate treatment."
The study appears in the current issue of the Journal of the American Medical Association. Matthew D. Barber, M.D., of the Cleveland Clinic in Ohio, led the study. Other authors were from institutions participating in the NICHD's Pelvic Floor Disorders Network. In addition to support from NICHD, the NIH Office of Research on Women's Health also provided funding.
Advertisement
After two years, the researchers evaluated the success of the surgical procedures and exercise course. The researchers judged success according to a scoring system that accounted for physician observations during a gynecological examination and the women's responses to questions about their symptoms. The scoring system took into account the extent to which the top of the vagina protruded into the vaginal canal, the need for follow-up surgery to treat the prolapse or urinary incontinence, and the women's experience of painful or bothersome sensations in the pelvic area.
Advertisement
In both surgical groups, the women experienced similarly low rates of serious adverse outcomes, with less than 5 percent having a serious adverse event directly related to the procedure.
The guided exercise program did not seem to offer additional benefit to most of the participants. Within both surgical groups, scores on measures of incontinence, prolapse and discomfort did not vary significantly between women in the exercise program and those who received usual care only. These results suggest that this supplemental exercise therapy may not be justified as routine care for all women who receive these two surgeries, the study authors wrote.
"It's helpful that we now know that, on the whole, these surgical techniques are very similar in the advantages they offer patients," Dr. Barber said. "Physicians skilled in both techniques can now tailor their surgical recommendations to each patient's individual case."
Source-Eurekalert










