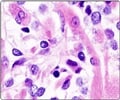
Geneticists led by University of Utah Nobel Prize Laureate Mario R. Capecchi, Ph.D., have engineered mice that develop clear cell sarcoma (CCS), a significant step
The rare and aggressive nature of sarcomas, and their occurrence in children and young adults, long has interested Capecchi. In a study in the Feb. 11, 2013, online edition of Cancer Cell, he and colleagues from the University of Utah, the University of Texas M.D. Anderson Cancer Center in Houston, and Stanford University, describe how they developed the first mouse model of CCS by essentially recreating the human ews-atf1 gene in mice.
Capecchi, distinguished professor of human genetics and a Howard Hughes Medical Institute Investigator, says having a mouse model will teach researchers not only about CCS but also might provide an avenue for developing a drug that is more successful than current therapies. "Now that we have a mouse model for CCS, we can investigate what other events or gene mutations are required to form tumors," he says. "It also gives us the opportunity to investigate whether the CCS fusion gene might be a specific target for drugs."
Sarcomas often are removed by surgery, which is followed by radiation or chemotherapy. If the fusion gene turns out to be a viable drug target, Capecchi cautions, it could take a decade or longer before it''s available to those with the disease.
Information from the National Cancer Institute estimated that 11,280 U.S. residents would be diagnosed with the disease in 2012, with approximately 3,900 people expected to die. Estimated mortality rates of CCS vary, but it is considered an aggressive cancer, with a five-year mortality rate of approximately 80 percent. In the United States, CCS accounts for around 7 percent of cancers among children, adolescents, and young adults under age 20, according to the National Cancer Institute.
To make the mouse model of CCS, Capecchi and his colleagues had to create the ews-atf1 fusion gene in mice. For this they employed the technique he developed and in 2007 was awarded the Nobel Prize in physiology or medicine for: gene targeting.
Advertisement
Although different cell types could give rise to this cancer, Capecchi identified mesenchymal stem cells, which can create a large number of tissue types, including the soft tissue where sarcomas form, as being especially good for producing CCS tumors. To activate the fusion gene, Cre must be injected into a mouse after birth.
Advertisement
"My feeling is that identifying the different steps that give rise to CCS tumors may be informative on how carcinomas develop." Capecchi says. "Sarcomas are genetically more stable than carcinomas, which makes it easier to identify the events leading to the cancer. Learning about CCS might shed light on carcinomas."
There are more than 20 types of sarcoma, each with a different fusion gene, according to Capecchi.
The first author on the study is Krystal M. Straessler, a graduate student in Capecchi''s lab. The other authors are Kevin B. Jones, M.D., and Huifeng Jin, both of the University of Utah orthopedics department and Hunstman Cancer Institute Center for Children''s Cancer; Hao Hu, University of Texas M.D. Anderson Cancer Center, Houston; Matt van de Rijn, Stanford University Medical Center, Palo Alto, Calif.
Source-Newswise