Higher body mass index is a risk factor for heart disease, but underweight patients were at higher risk for complications after revascularization using PCI.
‘After cardiac catheterization, patients with a lower body mass index had worse outcomes including readmission, length of stay, cost and mortality.’





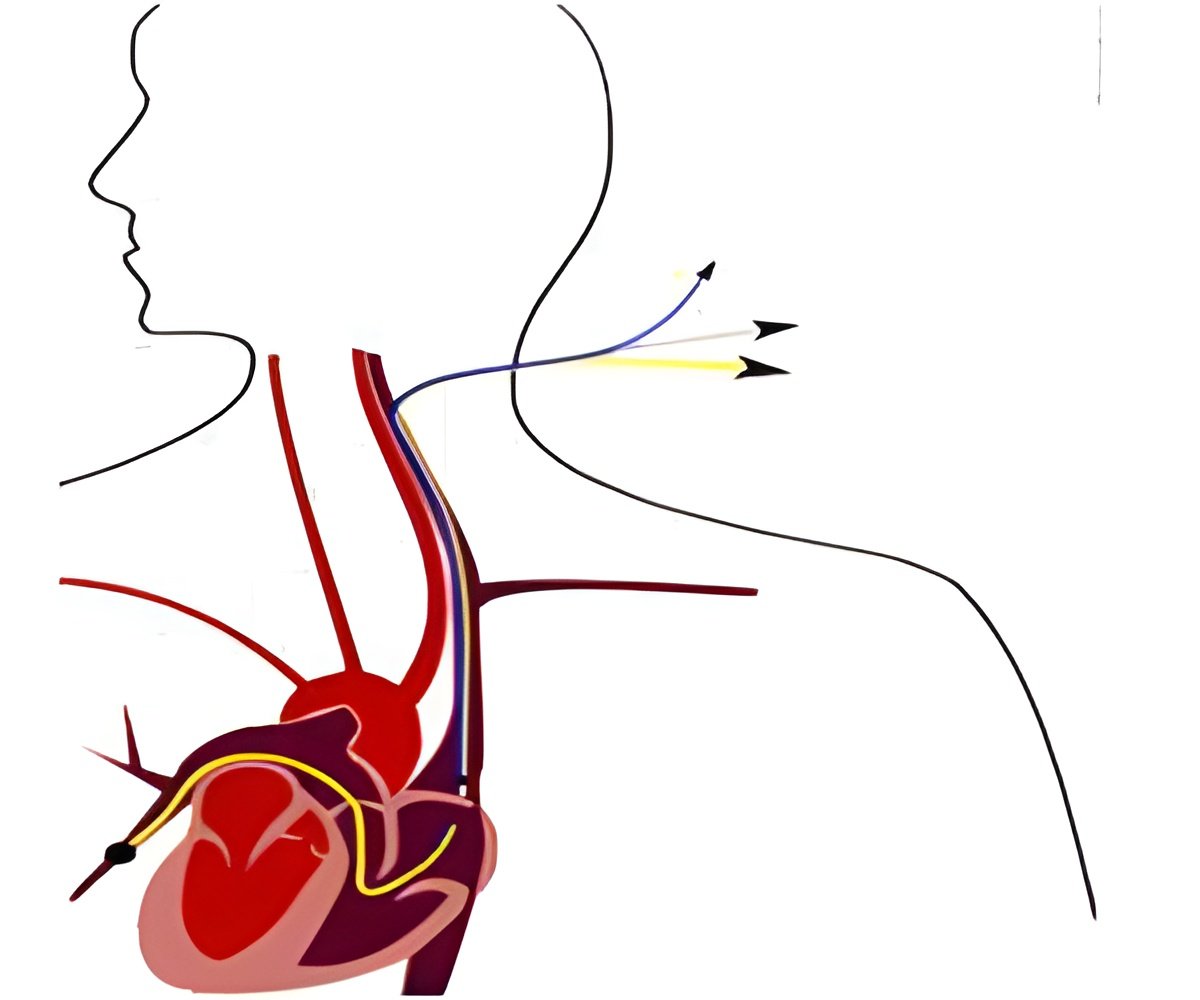
This study examined the association of BMI with in-hospital mortality, cost of care, length of stay, and rate of readmission within 30 days in patients undergoing cardiac catheterization (coronary angiography) in 2013 in a nationally representative cohort.Researchers used the National Readmission Database and Nationwide Inpatient Sample Database to retrospectively analyze discharge and readmission data. These are the largest all payer USA inpatient databases and include more than 35 million hospitalizations annually.
In 2013, 1 035 727 patients underwent cardiac catheterization, of which 42% also received PCI with a stent or balloon. When categorized by BMI, 0.4% of patients were underweight (BMI<19 kg/m2), while 11.4% were obese (BMI 30.1-40 kg/m2) and 8.0% were morbidly obese (BMI over 40 kg/m2). Of those undergoing cardiac catheterization, only 25.8% of the underweight patients went on to receive PCI, while 32.5% of the morbidly obese, 41% of the overweight, 41% of the obese, and 43.2% of the normal weight categories went on to have a balloon or stent (PCI) placed for coronary blockages (adjusted for co-morbidities: all values p<0.001).
Despite the low percentage of cardiac catheterizations and lower rate of PCI compared to normal and overweight BMI groups, underweight patients were over three times more likely to die after cardiac catheterization than morbidly obese patients and five times more likely to die than obese patients (6.0% mortality for underweight patients, 2.3% normal weight, 1.7% overweight, 1.2% obese, 1.9% morbidly obese, all values adjusted for co-morbidities: p<0.001). Interestingly, despite the extreme BMI, morbidly obese patients had a lower mortality rate than normal weight patients and obese patients had the lowest mortality of all groups undergoing cardiac catheterization.
Length of stay for underweight patients was more than double that of normal weight patients (10.5 days versus 5.1 days) resulting in nearly 50% higher costs for underweight patients ($USD 33 540 versus $USD 22 581). Morbidly obese patients had a slightly longer length of stay and higher costs compared to normal weight patients (6.2 days, p<0.01 and $USD 23 889, p<0.01).
Advertisement
Dr Tariq said: "The obesity paradox has flummoxed researchers for some time, and our research also flips the conventional wisdom that a higher BMI should portend a worse outcome. We found that the lower BMI group had worse outcomes across the board, including readmission, length of stay, cost, and mortality."
Dr Tariq concluded: "Further research will certainly add to the growing body of evidence, but the scales seem to be tipping in favor of higher BMI patients having better outcomes than normal weight patients. This study also reinforces the notion that the frail, those with the lowest BMI, have the worst outcomes - suggesting that when it comes to cardiac catheterization, the smaller they are, the harder they fall."
Source-Eurekalert