Presence of specific genetic mutations in young women is correlated with treatment-resistant breast cancer, whereas older women do not demonstrate the same link.

Molecular portraits of cell cycle checkpoint kinases in cancer evolution, progression, and treatment responsiveness
Go to source). The study's findings have implications for precision medicine and may introduce a novel approach to classifying breast cancer.
‘Certain genetic mutations in young women have been identified as risk factors for treatment-resistant breast cancer, while the same mutations do not exhibit a similar association in older women. These findings have potential implications for precision medicine and offer insights into a novel classification method for breast cancer.
# Breast Cancer, #Women, #Genetic Mutation
’





Advertisement
Beyond Age: Unraveling the Genetic Factors
“It’s well established that as you get older, you’re more likely to develop cancer. But we’re finding that this may not be true for all cancers depending on a person’s genetic makeup,” says senior author Svasti Haricharan, Ph.D., an assistant professor at Sanford Burnham Prebys.“There may be completely different mechanisms driving cancer in younger and older people, which requires adjusting our view of aging and cancer.”
The research primarily focused on ER+/HER2- breast cancer, which is one of the most common forms of the disease.
It is usually treated with hormonal therapies, but for some patients, these treatments don’t work. About 20% of tumors resist treatment from the very beginning, and up to 40% develop resistance over time.
“Understanding how certain forms of breast cancer develop in a way that makes them eventually resist therapy can help us better classify the disease. It may also help clinicians adjust the treatment plans for patients who will likely experience resistance to standard treatments,” says Haricharan. “For scientists like myself, it can help guide research to develop new therapies to overcome these obstacles.”
Advertisement
New Chapter in Precision Medicine
The study included an extensive analysis of a large database of breast cancer patients. It revealed that in ER+/HER2- breast cancer patients, certain gene mutations had a strong correlation with response to treatment —and the effects were dependent on age. Some gene mutations were only linked with treatment-resistant breast cancer in younger women.“This was a strange finding, so much so that we almost didn’t believe it at first,” says Haricharan. “But the same patterns emerged over and over again in database after database.”
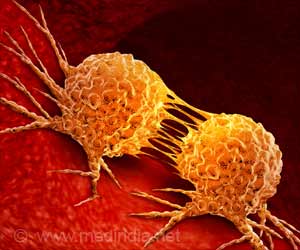
The mutations the researchers identified were in genes involved in cell replication, the process by which cells grow and divide. These genes are responsible for repairing mistakes when they happen—a process that goes awry in virtually all cancers.
“Cell cycle dysregulation occurs so early in the development of cancer that we generally don’t consider whether the individual mutations that cause cell cycle dysregulation can affect cancer’s eventual response to treatment or its ability to spread,” says Haricharan.
By connecting the specific type of cell cycle dysregulation that triggers cancer with the outcome of the disease many years after diagnosis, the research team proposes an entirely new paradigm for thinking about and studying all types of cancer.
Advertisement
Reimagining Breast Cancer Classification
“This is a radical shift in how we look at cancer, which could have implications well beyond breast cancer,” adds Haricharan.To begin to test this idea, the researchers analyzed the effect of cell cycle mutations on patient outcomes in other types of cancer.
In a final twist, they observed that across many cancer types, the mode of cell cycle dysregulation is significant for cancer in women, but less so for cancer in men. This suggests that the influence of cell-cycle dysregulation could depend on sex as well as age.
“These findings emphasize why it is important to study cancer in the context of the life history of the patient,” adds Haricharan. “Too often, cancer research is focused narrowly on cells in a petri dish, forgetting the whole, complex host system in which these cells transform and grow.”
Reference:
- Molecular portraits of cell cycle checkpoint kinases in cancer evolution, progression, and treatment responsiveness - (https://www.science.org/doi/10.1126/sciadv.adf2860)
Source-Eurekalert