Treatment at hospitals with higher rates of missed nursing care linked with black older adults being at a higher risk of repeat hospital admission after a heart attack.

‘Treatment at hospitals with higher rates of missed nursing care may be a contributing factor for black older adults being at a higher risk of repeat hospital admission after a heart attack.’





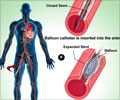
"Our findings suggest that unmet nursing care varies widely across US hospitals and that older blacks disproportionately receive care in settings where care is missed more often," comments lead author J. Margo Brooks-Carthon, of University of Pennsylvania School of Nursing's Center for Health Outcomes and Policy Research. "As the nation continues to intensify efforts to reduce health disparities, solutions may lie in ensuring adequate resources to nurses working in direct care." The researchers analyzed data on more than 69,000 black and white patients with acute myocardial infarction (AMI) treated at 253 hospitals in three states during 2006-07. Each hospital was classified in terms of how often necessary nursing care tasks were left incomplete due to a lack of time.
The study looked at differences in the characteristics of hospitals where black versus white patients were treated, including whether nursing care needs were unmet 'rarely, sometimes, or frequently'. This measure of unmet nursing care was also analyzed as a risk factor for repeat hospital admission within 30 days after AMI.
On average, black patients were younger but had more health problems than white patients; they also had lower socioeconomic status. Consistent with previous studies, the 30-day readmission rate was higher in black patients: 23.5%, compared to 18.8% in white patients.
"In general, older black patients were more often in hospitals where necessary care was omitted, and less often in the hospitals where care was rarely missed," says Dr. Brooks-Carthon. Unmet nursing care was associated with a higher risk of repeat admission for black patients, after adjustment for patient and hospital characteristics.
Advertisement
Surprisingly, some other types of unmet nursing care - such as discharge planning and patient education - were not significantly related to readmission risk. Unmet nursing care did not influence the likelihood of readmission for older white patients.
Advertisement
"Our findings suggest that older Black AMI patients endure greater consequences when nursing tasks are left incomplete," Dr. Brooks-Carthon- adds. The researchers conclude, "Any efforts to reduce readmission disparities must include investments to ensure that nurses who work on the front lines of care can attend to the complex social and healthcare needs of this population."
Source-Eurekalert