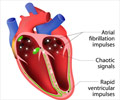
Treatment with electrical energy (radiofrequency ablation) resulted in lower rate of abnormal atrial rhythms and episodes of AF among patients with untreated paroxysmal atrial fibrillation.

Carlos A. Morillo, M.D., F.R.C.P.C., of McMaster University, Hamilton, Canada, and colleagues compared ablation to drug treatment as first-line therapy in patients with paroxysmal AF who had not previously received treatment. The trial included 127 patients at 16 centers in Europe and North America; 61 patients received antiarrhythmic drug treatment and 66 radiofrequency ablation.
Recurrence of an atrial tachyarrhythmia lasting longer than 30 seconds (the primary measured outcome) occurred more often in the antiarrhythmic drug group than in the ablation group, 44 patients (72 percent) vs. 36 patients (55 percent). Asymptomatic AF was also observed more frequently with drug treatment, 11 patients (18 percent) compared with 6 patients (9 percent). Symptomatic recurrence of abnormal rhythm was more common with drug treatment, 36 patients (59 percent) in the antiarrhythmic drug group compared with 31 patients (47 percent) in the ablation group.
Quality of life was improved overall by both treatments but not significantly different between groups. No deaths or strokes were reported in either group; 4 cases of cardiac tamponade (the accumulation of a large amount of fluid [usually blood] near the heart that interferes with its performance) were reported in the ablation group.
The authors conclude that recurrence of an atrial tachyarrhythmia was frequent in both groups, and that when offering ablation as a therapeutic option to patients with paroxysmal AF who have not previously received antiarrhythmic drugs, the risks and benefits need to be discussed and treatment strategy individually recommended. Available pre-embargo to the media at media.jamanetwork.com
Editor's Note: Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
Advertisement
Hugh Calkins, M.D., of Johns Hopkins Hospital, Baltimore, Md., comments on the findings of this study in an accompanying editorial.
Advertisement
Editor's Note: The author has completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Source-Eurekalert