An international research team, led by investigators from the Massachusetts General Hospital (MGH) Cancer Center and Dana-Farber Cancer Institute (DFCI), has found.
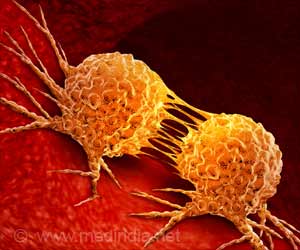
An international research team, led by investigators from the Massachusetts General Hospital (MGH) Cancer Center and Dana-Farber Cancer Institute (DFCI), has found a new way that some lung tumors become resistant to treatment with targeted therapy drugs like Iressa and Tarceva. Their report, which will appear in the journal Science and is receiving early online release, describes a totally new resistance mechanism that may apply to many types of cancer. It also suggests a treatment strategy for patients with these resistant tumors.
"We found that, for about 20 percent of patients with tumors that become resistant to Tarceva or Iressa, resistance is caused by the genetic activation of an oncogene that is not the normal target of the drug, which is something that has never been seen before," says Jeffrey Engelman, MD, PhD, scientific director of the MGH Center for Thoracic Cancers, the paper's lead author."Importantly, we also identified a potential new way to treat these resistant tumors with combination therapy directed against both protein targets," adds Pasi A. Jänne, MD, PhD, of the Lowe Center for Thoracic Oncology at DFCI, the study's senior author.
Drugs like Iressa (gefitinib) and Tarceva (erlotinib) are used to treat advanced non-small-cell lung cancer (NSCLC), the leading cause of cancer deaths in the U.S. They act by blocking the epidermal growth factor receptor (EGFR), a molecule on the surface of cancer cells. In 2004 research teams from MGH and DFCI found that only tumors in which the EGFR gene has been mutated in a way that magnifies the cells' response to the growth factor, a process that fuels tumor growth, were sensitive to treatment with these drugs.
Although tumors that respond to EGFR inhibitors do so rapidly and dramatically, eventually the tumors become resistant and resume growing. About half the time, a secondary mutation that interferes with the drugs' binding to the receptor develops within the EGFR gene. A new group of so-called irreversible EGFR inhibitors that permanently bind to the protein are currently being tested in clinical trials. But what leads to other cases of resistance has been unknown, and the current study was designed to discover additional mechanisms.
To do so, the investigators modeled in a laboratory setting what happens in lung cancer patients; they used a line of NSCLC cells with the sensitizing EGFR mutation and created a cell line resistant to treatment with Iressa. In a number of experiments comparing the resistant line with still-sensitive cells, they focused on the cell signalling pathway controlled by EGFR. In earlier research, Engelman and colleagues had found that the growth signal that starts with EGFR works through a related protein called ERBB3.
The current study showed that, in some of the resistant cells, ERBB3 is activated by amplification of a different oncogene called MET, in essence bypassing the blockage of EGFR. Analysis of samples from patients whose tumors became resistant after initially responding to Iressa revealed that MET was amplified in resistant samples from 4 of 18 patients. Although treating resistant cell lines with either Iressa or a MET inhibitor did not stop tumor growth, treatment with both agents did induce cell death.
Advertisement
"Our results suggest that, when patients' tumors become resistant, repeat biopsies to identify which resistance mechanism is involved will be critical and could help us develop effective therapies for those resistant tumors," adds co-author Lewis Cantley, PhD, of the Beth Israel Deaconess Medical Center.
Advertisement
Source-Eurekalert
MED/M