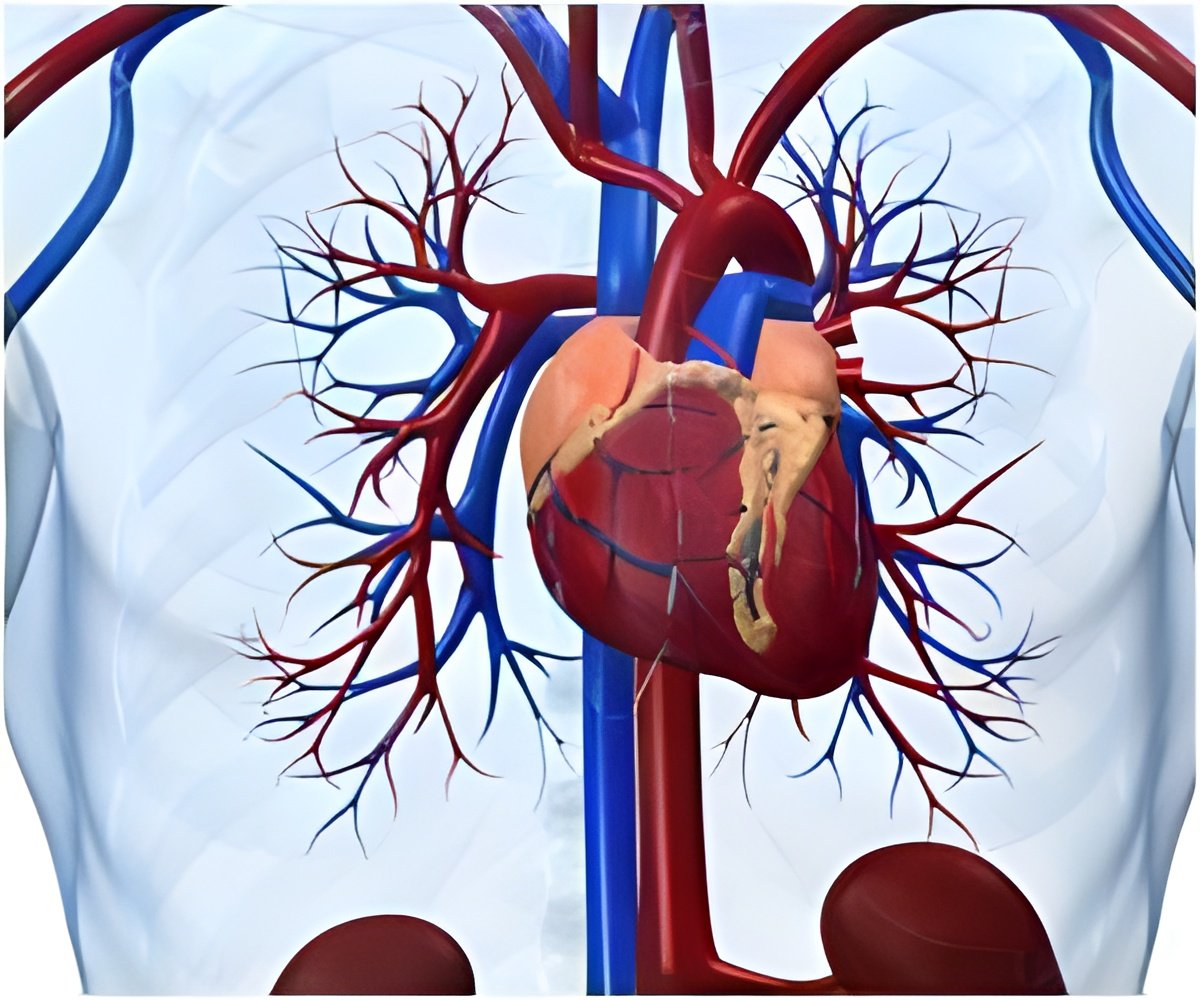
Among people with patent foramen ovale (PFO), a birth defect that causes a hole in the heart, medical devices that close the opening after a stroke have better results after two years compared to treatment with stroke-preventing medications alone.
‘According to this research, the use of medical devices to close the hole in patent foramen ovale (PFO) after a stroke may be more effective than taking stroke-preventing medications alone.’





Among patients younger than 55 years of age who experience a stroke of unknown cause, a cryptogenic stroke, the prevalence of PFOs has been found to be around 46 percent, much higher than the rate of PFOs in the general population. The new findings add to a growing body of evidence that closing the PFO after this type of stroke can help prevent subsequent strokes and related problems, particularly in those with a high-risk PFO. Researchers stopped enrollment for the trial early after determining, based on the results of several recent trials, that it would be unethical to continue assigning some patients to not receive the PFO closure device in light of mounting evidence of its clear benefits. Despite the smaller-than-expected number of participants, researchers said the new trial helps clarify which patients are likely to benefit most from the medical device based on the physical characteristics of their PFO.
"Considering the high prevalence of PFO in the general population and cryptogenic stroke patients, the key to appropriate use of this medical device is determining how to select optimal candidates for the procedure," said Jae Kwan Song, MD, a cardiologist at Asan Medical Center in Seoul, South Korea and the study's lead author. "Our study showed that the potential benefit from closure can be determined on the basis of the size of the PFO and the movement of the heart wall around the PFO."
The trial enrolled 120 patients at two centers in South Korea. All patients had recently experienced a cryptogenic stroke and were found to have a high-risk PFO, meaning either the PFO was 2 millimeters across (about the size of a peppercorn) or larger, or the PFO was accompanied by an outgrowth of tissue protruding into one of the heart's chambers.
All patients received medications such as anticoagulants or antiplatelet drugs, which are recommended after a stroke to reduce the formation of blood clots and prevent subsequent strokes. The specific type of medication was determined by each patient's physician, although no direct oral anticoagulants (also known as novel oral anticoagulants) were used in the study. Half of the patients were randomly assigned to receive a PFO closure device, which interventional cardiologists implanted in the heart by threading the device through a vein in the groin, while the other half received medications alone.
Advertisement
"We believe that PFO closure should be done in selected patients with cryptogenic stroke and PFO," Song said. "With our study and other recent trials, the criteria for selecting patients for the procedure are becoming clearer; in particular, the results suggest that closure is beneficial for those with high-risk PFO."
Advertisement
Source-Eurekalert









