A new study identifies the steady accumulation of a protein in healthy, aging brains as a probable cause of seniors' vulnerability to neurodegenerative disorders.
The pharmaceutical industry has spent billions of dollars on futile clinical trials directed at treating Alzheimer's disease by ridding brains of a substance called amyloid plaque. But the new findings have identified another mechanism, involving an entirely different substance, that may lie at the root not only of Alzheimer's but of many other neurodegenerative disorders — and, perhaps, even the more subtle decline that accompanies normal aging.
The study, to be published Aug. 14 in the Journal of Neuroscience, reveals that with advancing age, a protein called C1q, well-known as a key initiator of immune response, increasingly lodges at contact points connecting nerve cells in the brain to one another. Elevated C1q concentrations at these contact points, or synapses, may render them prone to catastrophic destruction by brain-dwelling immune cells, triggered when a catalytic event such as brain injury, systemic infection or a series of small strokes unleashes a second set of substances on the synapses.
"No other protein has ever been shown to increase nearly so profoundly with normal brain aging," said Ben Barres, MD, PhD, professor and chair of neurobiology and senior author of the study. Examinations of mouse and human brain tissue showed as much as a 300-fold age-related buildup of C1q.
The finding was made possible by the diligence and ingenuity of the study's lead author, Alexander Stephan, PhD, a postdoctoral scholar in Barres' lab. Stephan screened upward of 20,000 antibodies before finding one that binds to C1q and nothing else. (Antibodies are proteins, generated by the immune system, that adhere to specific "biochemical shapes," such as surface features of invading pathogens.)
Comparing brain tissue from mice of varying ages, as well as postmortem samples from a 2-month-old infant and an older person, the researchers showed that these C1q deposits weren't randomly distributed along nerve cells but, rather, were heavily concentrated at synapses. Analyses of brain slices from mice across a range of ages showed that as the animals age, the deposits spread throughout the brain.
Advertisement
Other scientists have observed moderate, age-associated increases (on the order of three- or four-fold) in brain levels of the messenger-RNA molecule responsible for transmitting the genetic instructions for manufacturing C1q to the protein-making machinery in cells. Testing for messenger-RNA levels — typically considered reasonable proxies for how much of a particular protein is being produced — is fast, easy and cheap compared with analyzing proteins.
Advertisement
C1q is the first batter on a 20-member team of immune-response-triggering proteins, collectively called the complement system. C1q is capable of clinging to the surface of foreign bodies such as bacteria or to bits of our own dead or dying cells. This initiates a molecular chain reaction known as the complement cascade. One by one, the system's other proteins glom on, coating the offending cell or piece of debris. This in turn draws the attention of omnivorous immune cells that gobble up the target.
The brain has its own set of immune cells, called microglia, which can secrete C1q. Still other brain cells, called astrocytes, secrete all of C1q's complement-system "teammates." The two cell types work analogously to the two tubes of an Epoxy kit, in which one tube contains the resin, the other a catalyst.
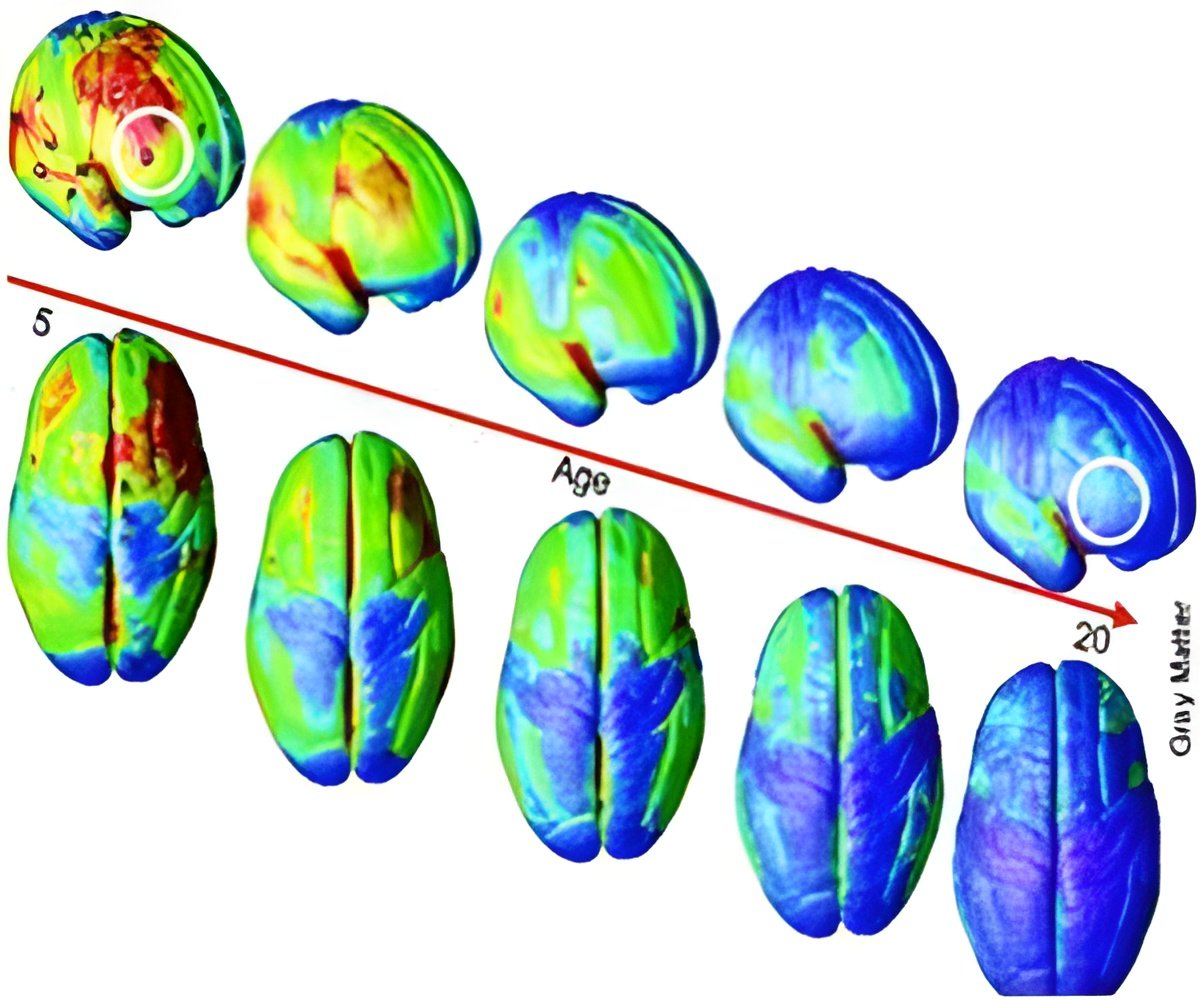
Previous work in Barres' lab has shown that the complement cascade plays a critical role in the developing brain. A young brain generates an excess of synapses, creating a huge range of options for the potential formation of new neural circuits. These synapses strengthen or weaken over time, in response to their heavy use or neglect. The presence of feckless connections contributes noise to the system, so the efficiency of the maturing brain's architecture is improved if these underused synapses are pruned away.
In a 2007 paper in Cell, Barres' group reported that the complement system is essential to synaptic pruning in normal, developing brains. Then in 2012, in Neuron, in a collaboration with the lab of Harvard neuroscientist Beth Stevens, PhD, they showed that it is specifically microglia — the brain's in-house immune cells — that attack and ingest complement-coated synapses.
Barres now believes something similar is happening in the normal, aging brain. C1q, but not the other protein components of the complement system, gradually becomes highly prevalent at synapses. By itself, this C1q buildup doesn't trigger wholesale synapse loss, the researchers found — although it does seem to impair their performance. Old mice whose capacity to produce C1q had been eliminated performed subtly better on memory and learning tests than normal older mice did.
Still, this leaves the aging brain's synapses precariously perched on the brink of catastrophe. A subsequent event such as brain trauma, a bad case of pneumonia or perhaps a series of tiny strokes that some older people experience could incite astrocytes — the second tube in the Epoxy kit — to start secreting the other complement-system proteins required for synapse destruction.
Most cells in the body have their own complement-inhibiting agents. This prevents the wholesale loss of healthy tissue during an immune attack on invading pathogens or debris from dead tissue during wound healing. But nerve cells lack their own supply of complement inhibitors. So, when astrocytes get activated, their ensuing release of C1q's teammates may set off a synapse-destroying rampage that spreads "like a fire burning through the brain," Barres said.
"Our findings may well explain the long-mysterious vulnerability specifically of the aging brain to neurodegenerative disease," he said. "Kids don't get Alzheimer's or Parkinson's. Profound activation of the complement cascade, associated with massive synapse loss, is the cardinal feature of Alzheimer's disease and many other neurodegenerative disorders. People have thought this was because synapse loss triggers inflammation. But our findings here suggest that activation of the complement cascade is driving synapse loss, not the other way around."
In 2011, Barres co-founded a company, Annexon, to develop drugs that inhibit the complement cascade to treat Alzheimer's, glaucoma, Parkinson's, stroke, multiple sclerosis and several other neurodegenerative diseases characterized by massive synapse loss. Annexon has licensed multiple associated patent applications from Stanford, which filed them.
Other Stanford co-authors of the study were Daniel Madison, PhD, associate professor of molecular and cellular physiology; Mehrdad Shamloo, PhD, associate professor of comparative medicine; postdoctoral scholars Laurence Coutellier, PhD, and Jose Maria Mateos, PhD; research associate Emilie Lovelett; and graduate student Dominic Berns.
Source-Eurekalert














