The respiratory deterioration in adults infected with COVID-19 is immune-mediated and not directly related to viral replication. The severity of infection was reduced in children as they have higher levels of T-cells, that have an immune modulator response and thus prevent the virus.
‘In the U.S, only around 1.7% of the first 149,082 cases were infants, children, and adolescents younger than 18. The immune system in children responds to viruses differently from adults, causing less severe illness in pediatric patients.’





The study by pediatric and adult physicians at The University of Texas Health Science Center at Houston (UTHealth) and Baylor College of Medicine, is published in the American Journal of Physiology-Lung Cellular and Molecular Physiology.According to the paper, only about 1.7% of the first 149,082 cases in the U.S. were infants, children, and adolescents younger than 18 years old. Authors noted that children under 18 make up 22% of the U.S. population. Only three pediatric deaths were identified by the Centers for Disease Control and Prevention (CDC) as of April 2020.
"These profoundly decreased rates of symptomatic infection, hospitalization, and death are well beyond statistical significance, require further examination, and may hold the key to identifying therapeutic agents," the authors wrote.
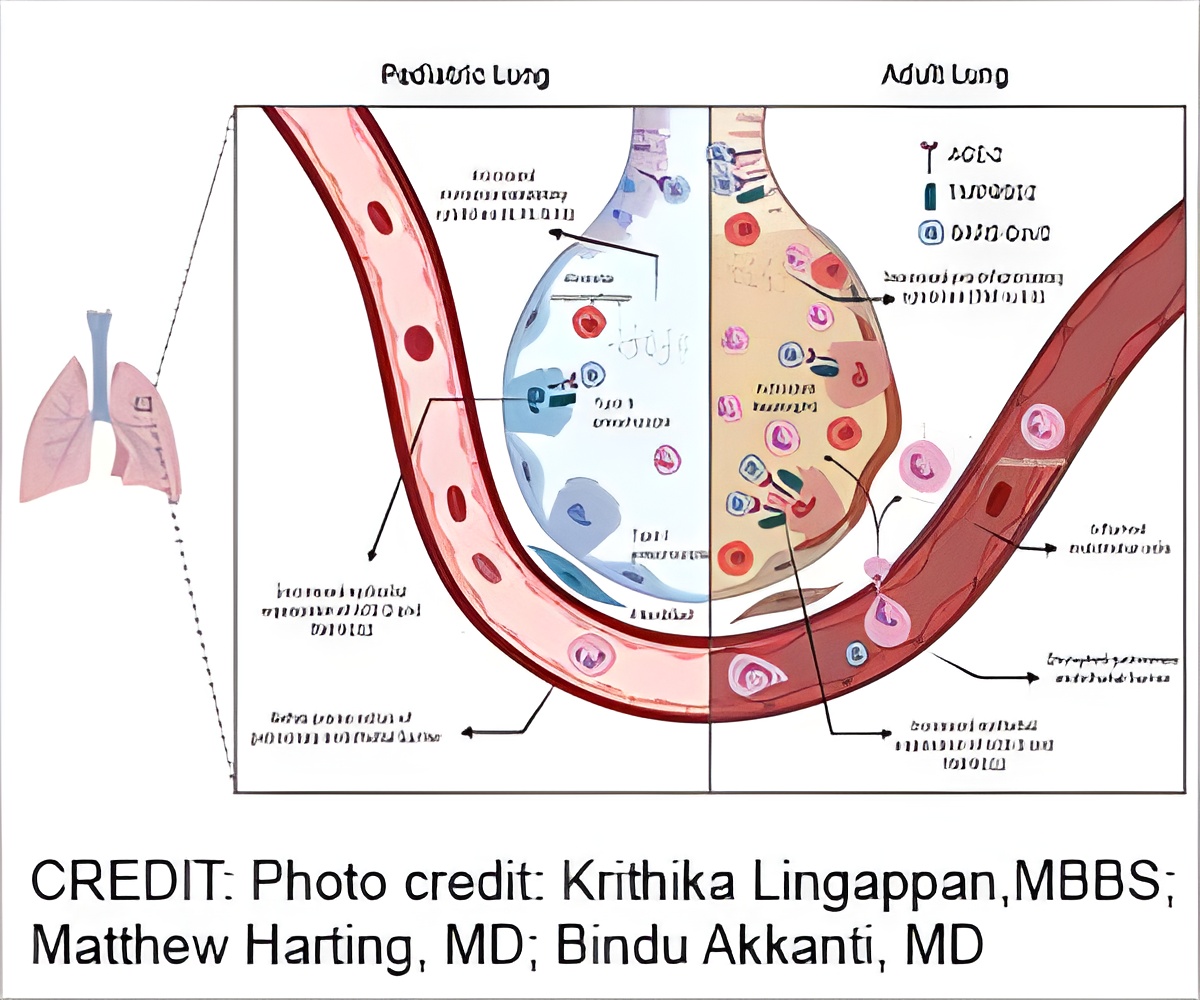
Angiotensin-converting enzyme 2s, called ACE2, are the doors that allow SARS-CoV-2, the novel coronavirus that causes COVID-19, to enter the body's cells. Children naturally have less ACE2 in the lungs than adults.
"ACE2 are important for viral entry and there seems to be less of them in children, because they increase with age," said Matthew Harting, MD, MS, assistant professor in the Department of Pediatric Surgery at McGovern Medical School at UTHealth, pediatric surgeon with UT Physicians, and senior author of the paper. Harting is also director of the pediatric ECMO program providing advanced cardiac and respiratory support at Children's Memorial Hermann Hospital.
Advertisement
"T-cells have a viral response and also an immune modulator response. In severe cases of adult COVID-19 patients, we've seen that those T-cells are reduced, so the ability to fight the virus is also reduced. In kids, those T-cells seem to be maintained, so they are still able to prevent the virus," said Harry Karmouty-Quintana, PhD, an assistant professor in the Department of Biochemistry and Molecular Biology at McGovern Medical School, and a co-author of the paper.
Advertisement
"IL-10 inhibits the inflammation of other components like IL-6 that are detrimental. Adults tend to experience hyperinflammatory state, where kids do not," Karmouty-Quintana said. "In preclinical studies in mice, IL-10 has also shown to decrease with age."
The paper's findings were made possible through collaboration in a multidisciplinary group made up of pediatric and adult physicians and scientists in pediatric surgery, adult critical care, neonatology, and molecular biology.
"We, as physicians, have been challenged with the question of how to treat COVID-19 and we're learning in real time," said Bindu Akkanti, MD, associate professor of critical care medicine with McGovern Medical School, attending physician in critical care with Memorial Hermann-Texas Medical Center, and a study co-author. "I knew that to figure out the best way to treat adults, we needed to get a team together to get to the bottom of why children were being spared from severe illness related to the virus. So, I reached out to Dr. Karmouty-Quintana and we teamed up with Dr. Harting and two other physicians in the Texas Medical Center to start investigating." Akkanti also sees pulmonary patients at UT Physicians.
"Collaborations like this between adult and pediatric providers are really important and this disease highlights where we can learn a lot when we compare the way it behaves in younger kids with older people," Harting said. "Even now as we're learning about effective treatments, we're seeing younger people handle this disease better than older people. Moving forward, physicians and scientists need multidisciplinary collaboration to continue learning - this is just another step in the right direction to attack this virus."
Krithika Lingappan, MBBS, was the first author of the paper and Jonathan Davies, MD, was a co-author. Both Lingappan and Davies are assistant professors of pediatrics at Baylor College of Medicine and neonatologists with Texas Children's Hospital.
As a result of the collaboration, the team has begun a new study using blood samples from patients in different stages of COVID-19 to continue to understand how to treat the virus and the disparities in disease progression between children and adults.
Source-Eurekalert















