Patients who don't respond to treatments that use their own immune cells to destroy tumors share changes in mechanisms that switch genes on or off in those cells.

‘A pattern of 'gene dysregulation' causes immune T cells to turn back to an immature state, making the cells less effective against metastatic melanoma.’





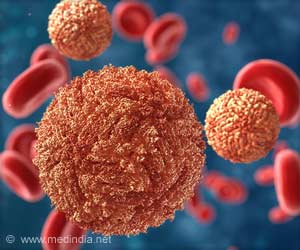
Patients who don't respond to treatments that use their own immune cells to destroy tumors, called tumor infiltrating lymphocytes, share changes in mechanisms that switch genes on or off in those cells, revealed study results presented at the annual meeting of the American Society for Clinical Oncology (ASCO). Led by researchers from NYU Langone Medical Center and its Laura and Isaac Perlmutter Cancer Center, the study found that a pattern of 'gene dysregulation' causes immune T cells to turn back to an immature state, making the cells less effective against metastatic melanoma, a deadly form of skin cancer. Such 'immunotherapies' work by enhancing, not disrupting, the ability of T cells to identify and destroy cancer cells the way they would an invading virus.
"Our research offers key evidence for genetic and epigenetic dysregulation as a reason these powerful immune therapies fail to work for so many people with widespread melanoma," says study senior investigator and medical oncologist Jeffrey Weber, deputy director of the Perlmutter Cancer Center and a professor at NYU Langone. The NYU Langone team performed the study in collaboration with colleagues at the Moffitt Cancer Center in Tampa, Fla.
Weber says treatment with immune-based therapies in recent decades has increased the number of people with advanced melanoma who survive longer than five years from 10% to 30%, or more. Many immunotherapies still fail, however, with part of the problem attributed to tumor cells suppressing the T cell populations that enable immunotherapy. Factors involved in regulating gene activity tied to T cell function also were figured to play a role in treatment failure, and the new research sought to find out more about those.
The current study results are based on an analysis of the genes in 24 melanoma patients. Researchers searched for patterns of changes in the epigenome, or chemical modifications to the DNA code that assist in controlling which genes are turned on and which genes are turned off.
Advertisement
Researchers found more than 60 epigenetic changes as well as 10 changes in gene activity that were most common to people for whom immunotherapy failed. Many of these changes were known from previous research to control the process by which immature cells become either CD4 or CD8 immune T cells. Both are essential in immunotherapy in recognizing and attacking cancer cells, says Weber, who proposes that these changes lead to T cell malfunction.
Advertisement
"If our research is confirmed, it suggests that by modifying the genetic or epigenetic alterations we have identified, we can potentially turn treatment non-responders into responders and broaden the success that immunotherapies are having against melanoma and other cancers," says study lead investigator David Woods, PhD, a postdoctoral fellow at NYU Langone.
Moreover, Woods says these proposed, corrective actions would have an added advantage in that they could be performed in the patients' T cells while the cells are grown in the lab and before the cells are injected into any patient, presenting a potentially safe and convenient treatment option. A patient's T cells can be replicated quickly in lab cultures, with as many as 100 billion cells produced within a few weeks.
Reprogramming dysfunctional T cells while they grow, Woods says, might help increase the effectiveness of immunotherapy, particularly when the new T cells are infused back into the patients in combination with other approved, immune-boosting agents like interleukin-2 or checkpoint inhibitors.
Source-Eurekalert