Is advanced bladder cancer treatable? Advanced bladder cancer is hard to treat. Despite, aggressive treatment with surgery, chemotherapy, and radiation, most bladder cancer patients don’t get it.
‘Is advanced bladder cancer treatable? Advanced bladder cancer is hard to treat. Despite, aggressive treatment with surgery, chemotherapy, and radiation, most bladder cancer patients don’t get it.’
Read More..




Why doctors are not treating these patients with an intent to cure is complicated. But UC Davis Health Distinguished Professor Emeritus Ralph de Vere White, first author on a paper published in Journal of Clinical Oncology, argues it’s a problem that can – and must – be solved.Read More..
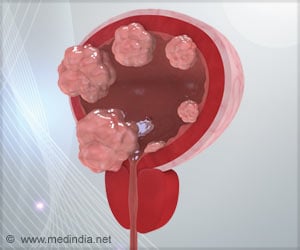
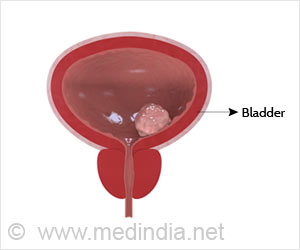
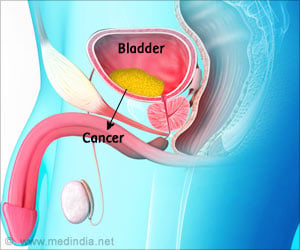
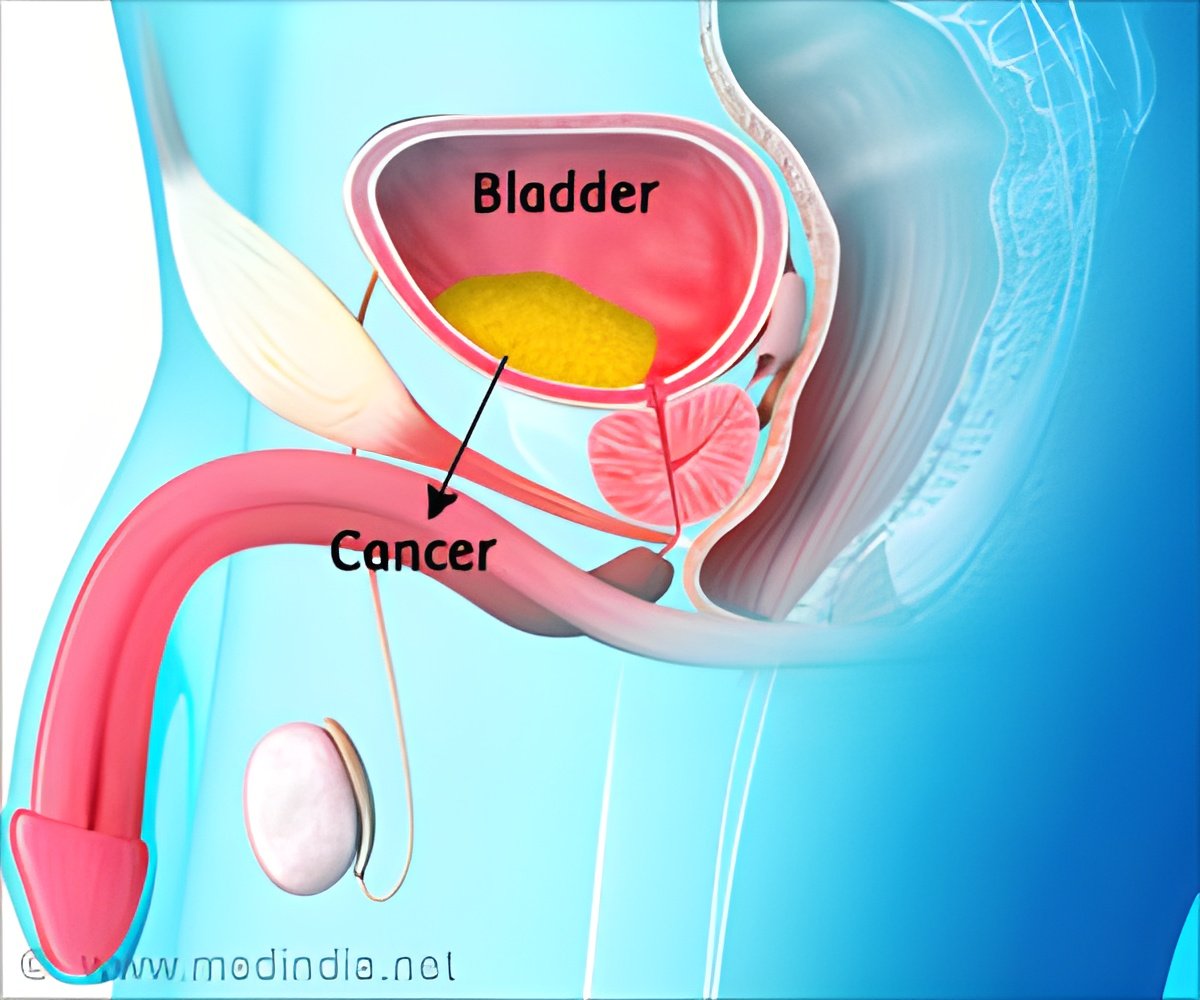
The paper, which has been endorsed by the Society of Urologic Oncology, is focused on the 25% of bladder cancers that grow outside the lining of the bladder and into the muscle wall, called muscle-invasive bladder cancer, or MIBC. These cancers are harder to treat and more likely to spread outside of the bladder and into lymph nodes or other organs. They account for the vast majority of bladder cancer mortality in the U.S., about 17,000 deaths per year.
De Vere White and his co-authors examined data from multiple studies and concluded that more than half of the MIBC patients receive no treatment with an intent to cure their disease. These treatments would be chemotherapy followed by a complete surgical bladder removal, also called a cystectomy.
Another approach would be a transurethral resection of the bladder, a less invasive procedure in which a surgeon uses instruments to look inside the bladder and remove tumors, plus chemotherapy and radiation treatment, also called trimodal therapy.
The 5-year survival rate for bladder cancer patients has remained unchanged at about 35% for decades, and yet recent studies show much better survival for bladder cancer patients who receive treatment with an intent to cure. One 2018 study, for example, showed 79% of patients survived at least 10 years after radical cystectomies and 69% survived at least 10 years after tri-modal therapy.
Advertisement
Why so few patients get treated relates, in large part, to the fact that cystectomy is a costly and complex surgery that can result in complications and lead to emergency room visits, hospital readmission and death. Many patients also don’t want or cannot afford to travel long distances to centers that perform the operation, and their local hospitals or clinics don’t want to deal with post-operative complications. In addition, the authors write, “there may be considerable confusion among urologists, radiation therapists and medical oncologists on how best to select patients” for the optimal treatment approaches.
Advertisement
“I think it’s a perfect storm,” said de Vere White, adding that bladder cancer is on the rise due to the aging population. Smoking is also major risk factor for the disease.
“We need to find out what the problem is,” he said. “We need doctors and patients to understand that at this time many patients are not receiving treatment that could prolong their life, and we need to find out why.”
De Vere White and his co-authors suggest that the hospitals and health systems considered bladder cancer “centers of excellence” partner with smaller centers, community practices and individual providers to ensure their patients receive the most effective therapy possible. This approach, endorsed by the Society of Urological Oncology, should be led by an interdisciplinary team from various national urology, medical oncology and radiation oncology professional organizations.
Other authors on the paper include Primo N. Lara, Jr., Christopher P. Evans and Marc Dall’Era, of UC Davis Health and Peter C. Black of Vancouver Prostate Centre at the University of British Columbia.
Source-Newswise