Research from the Stanford University School of Medicine has revealed that the window to treat stroke patients may just be a little longer than earlier anticipated
Research from the Stanford University School of Medicine has revealed that the window to treat stroke patients may just be a little longer than earlier anticipated.
If a patient arrives at the emergency room within three hours of experiencing stroke symptoms, doctors can administer a potent clot-busting medication and often save critical brain tissue. But if more than three hours have passed, current clinical guidelines say the medication should not be used.But the new study suggests that the traditional three-hour time window is too short. By combining data from multiple clinical trials, Maarten Lansberg, MD, PhD, assistant professor of neurology and neurological sciences at Stanford, and colleagues from Belgium and Germany showed that treatment can benefit patients up to 4.5 hours after they experience their first symptom. Their findings will be published online May 28 in the journal Stroke.
Every year, more than 750,000 Americans experience a stroke, or brain attack, due to a sudden drop in blood flow to the brain. Most strokes are ischemic, meaning they're caused by a blocked artery. For these strokes, a medication called tissue plasminogen activator, or tPA, can open blocked blood vessels and help restore blood flow to the brain.
"We've known that this treatment works for ischemic stroke since 1995," said Lansberg, the lead author of the study. "But in the United States, only about 3 percent of stroke patients end up getting treated. Most of them are ineligible because they come to the hospital after the three-hour time window."
The timing of treatment is important, because giving a strong blood thinner like tPA during a stroke can cause bleeding inside the brain. The longer a patient waits to get treatment, the more likely it is that the risks of treatment will outweigh the benefits.
"Doctors from all over the world have tried to increase the treatment time window," Lansberg said. But evidence from individual clinical trials has been confusing: Some studies demonstrated a benefit from treatment after three hours, while others were inconclusive or reported no benefit.
Advertisement
But when Lansberg and colleagues combined data from all four of the major tPA stroke trials to date, they saw a much clearer picture. Among a total of 1,622 patients who arrived at the hospital between three and 4.5 hours after their symptoms started, treatment with tPA improved the odds of a favorable outcome by 31 percent.
Advertisement
The study, funded by grants from the National Institutes of Health, found no change in the death rate among patients treated with tPA during the three- to 4.5-hour window. In other words, treatment improved outcomes without negatively affecting mortality.
Lansberg collaborated with Vincent Thijs, MD, PhD, professor of neurology at the University Hospitals of Leuven in Belgium, and Erich Bluhmki, PhD, who works for Boehringer Ingelheim Pharma GmbH & Co. Boehringer Ingelheim manufactures tPA for use in Europe.
A second study, also led by Lansberg and published online in Stroke on April 16, further supports these findings. Using data from six previous trials, the researchers calculated the likelihood that patients would benefit or be harmed by tPA treatment. Out of 100 patients treated three to 4.5 hours after the onset of stroke, the study estimated 16.9 patients would benefit and only 3.4 would be harmed.
"Although this is not as good as treatment at an earlier time, it is still a highly significant benefit for patients treated in this group," Lansberg said.
Stanford doctors have already started to incorporate the new data into their clinical decision-making, Albers said. Although the FDA has not approved tPA for use more than three hours after the onset of symptoms, physicians can offer the treatment to patients as an "off-label" use.
"Until these data came out, we were treating patients up to three hours," Lansberg said. "Now, after carefully explaining the risks and benefits, we give patients the option to get treatment up to 4.5 hours after their symptoms start."
Albers estimates that roughly 15 percent of patients at Stanford come in during the three- to 4.5-hour time window. "It varies by location," he said, "because if you live in a remote area, you're less likely to get to the hospital in time. But with 750,000 strokes happening every year in the United States, it's quite a large number of patients who could potentially benefit."
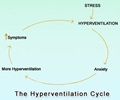
Despite a longer window for treatment, Lansberg stressed the classic mantra of stroke researchers: "'Time is brain' still holds true," he said. "When your brain doesn't get the sugar and oxygen it needs, your brain cells die. For every minute you wait, your chances of getting better from the treatment drop."
Source-Eurekalert
RAS