Over the following 11 years, women aged 50 or younger who suffer a heart attack are more likely than men to die, found a new study.
‘Women with a heart attack or to be treated with specific medical therapies upon discharge, such as aspirin, beta-blockers, ACE inhibitors, and statins, are less likely to undergo therapeutic invasive procedures after hospital admission. ’





Researchers analyzed 404 women and 1693 men who had a first heart attack (a myocardial infarction) between 2000 and 2016. The participants' median age was 45, and 53% of study participants had ST-elevation myocardial infarction (STEMI). The patients were treated at the Brigham and Women's Hospital and Massachusetts General Hospital in the US. STEMI is a type of heart attack where there is a prolonged interruption to the blood supply caused by a total blockage of the coronary artery.
Women were less likely than men to have STEMI (46.3% versus 55.2%), but more likely to have non-obstructive coronary disease. Chest pain was the most common symptom observed in both men and men.
Prof. Blankstein said: "Among patients who survived to hospital discharge, there was no significant difference in deaths from cardiovascular problems between men and women. Cardiovascular deaths occurred in 73 men and 21 women, 4.4% versus 5.3% respectively, over a median follow-up time of 11.2 years. However, when excluding deaths that occurred in hospital, there were 157 deaths in men and 54 death in women from all causes during the follow-up period: 9.5% versus 13.5% respectively, which is a significant difference, and a greater proportion of women died from causes other than cardiovascular problems, 8.4% versus 5.4% respectively, 30 women and 68 men. After adjusting for factors that could affect the results, this represents a 1.6-fold increased risk of death from any cause in women."
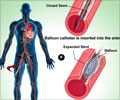
Women were less likely to undergo invasive coronary angiography (93.5% versus 96.7%).
Advertisement
Prof. Blankstein added: "As fewer women had STEMI and more had non-obstructive myocardial infarction, they are less likely to undergo coronary revascularisation or to be given medications such as dual anti-platelet therapy, which is essential after invasive heart procedures. Also, the absence of obstructive coronary artery disease may raise uncertainty regarding the diagnosis and whether such individuals truly had a myocardial infarction or have elevated enzymes due to other causes."
Advertisement