- Acute Coronary Syndrome: Current Treatment - (http://www.aafp.org/afp/2017/0215/p232.html)
- Heart Disease: Symptoms, Diagnosis, Treatment - (https://medlineplus.gov/magazine/issues/winter09/articles/winter09pg25-27.html)
- FACTORS IMPORTANT FOR THE GROWTH OF HISTOPLASMA CAPSULATUM IN THE YEAST CELL PHASE ON PEPTONE MEDIA I. - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc3861005/)
- Acute Coronary Syndrome - (https://www.heart.org/heartorg/conditions/heartattack/aboutheartattacks/acute-coronary-syndrome_ucm_428752_article.jsp)
- Acute Coronary Syndromes: Diagnosis and Management, Part I - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc2755812/)
- New oral anticoagulants in addition to single or dual antiplatelet therapy after an acute coronary syndrome: a systematic review and meta-analysis - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc3675388/)
- Developments in the invasive diagnostic–therapeutic cascade of women and men with acute coronary syndromes from 2005 to 2011: a nationwide cohort study - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc4466619/)
- Cardiac CT: atherosclerosis to acute coronary syndrome - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc4278045/)
What is Acute Coronary Syndrome?
Acute coronary syndrome (ACS) is a sudden and life-threatening condition caused by a sudden reduction in blood flow to the heart. The incidence of coronary disease in Indians who are 55-60 years old is 50% and about 25% in those who are less than 40 years old.
In the United States, an ACS occurs every 25 seconds, and an ACS-related death occurs every minute. Each year in the USA, approximately 1.4 million patients are hospitalized for ACS.
Modern fast paced lifestyle, increased incidence of diabetes; obesity and hypertension have been attributed for the high rates of acute coronary syndrome.
ACS is an umbrella term which includes unstable angina (UA), ST segment elevation myocardial infarction (STEMI) and non ST-segment elevation myocardial infarction (NSTEMI). These are caused by narrowing and acute blood clots in the coronary arteries. This is mostly due to rupture of an atherosclerotic plaque which can produce partial or complete blockage of the artery.
- Unstable angina is a potentially serious condition characterized by persistent chest pain. This angina does not usually respond to rest or medication. It may be a precursor to a heart attack.
- ST segment elevation myocardial infarction (STEMI) is the most severe form of ACS. The "ST segment" on the ECG is elevated when a coronary artery is completely blocked and a large proportion of the heart muscle begins to die.
- Non ST-segment elevation myocardial infarction (NSTEMI) occurs when the blockage in the coronary artery is only partial and the damage is lesser than STEMI. This is also known as non “Q” wave myocardial infarction.
What are the Causes of Acute Coronary Syndrome?
Acute coronary syndrome is caused by coronary artery disease due to atherosclerosis and hardening of arteries. This is from the buildup of fatty deposits (plaques) in the walls of coronary arteries, the blood vessels delivering oxygen and nutrients to heart muscles. This causes a narrowing of the arteries and slowing or blockage of the blood flow to the heart.
When a plaque deposit ruptures or detaches, a blood clot forms. This clot obstructs the flow of blood to heart muscles causing reduced oxygen supply. This results in unstable angina or a complete blockage resulting in myocardial infarction (heart attack).
What are the Signs and Symptoms of Acute Coronary Syndrome?
- Pain, discomfort in the chest or radiating from the chest to the shoulders, arms, upper abdomen, back, neck and jaw. The pain may be described as tightness, pressure, aching or burning in the chest. This is the most common symptom associated with ACS
- Fast and irregular heartbeat
- Extreme anxiety, feeling of impending doom
- Shortness of breath
- Feeling dizzy, lightheaded or fainting
- Cold and clammy skin due to sudden, heavy sweating (diaphoresis)
- Nausea or vomiting
- Indigestion
- Unexplained fatigue

How do you Diagnose Acute Coronary Syndrome?
The followings tests are performed to aid in the diagnosis of ACS.
- Electrocardiogram (ECG) is performed to measure the electrical activity of the heart via electrodes attached to the skin. Studies suggest that patients with no ECG changes are at a lower risk of complications than those with ECG changes.
- Echocardiogram is a non invasive test which uses sound waves to produce live images of the heart. An echocardiogram may also be used as part of an exercise stress test, to detect the location and extent of heart muscle damage.

- Coronary angiogram is an invasive test which uses X-ray imaging to see the blood vessels of the heart. A catheter is threaded through an artery in the arm or groin, up to the heart. A liquid dye is then injected and multiple X-ray images of the heart taken can reveal blockage or narrowing of the arteries.
- Computed tomography angiography (CTA) is a heart-imaging test that uses CT technology and iodine-rich contrast dye to visualize the heart anatomy, coronary circulation, the aorta, pulmonary veins, and arteries. CTA scanning helps to diagnose and evaluate blood vessel disease, aneurysms or blockages.
- Stress test assesses how well the heart functions during exercise. This test is done when there is no evidence of cardiac abnormality during rest.
- Myocardial perfusion imaging (MPI) is an imaging technique widely used for diagnosis, staging of disease and follow-up whileexposing the body to a low-dose ionizing radiation. A small amount of radioactive isotope such as thallium or technetium is injected into the patient's vein. The radioactive isotope attaches to red blood cells and can then be traced through the heart using special scanners.
- Blood tests for biologic markers
Troponins and creatine kinase myocardial band (CK-MB). They are released into the bloodstream when heart cells become damaged.
Biomarkers such as myeloperoxidase and glycogen phosphorylase isoenzyme-BB are early markers of ACS even before the occurrence of symptoms.
How do you Treat Acute Coronary Syndrome?
The initial management of UA/NSTEMI involves both aggressive medical therapy and revascularization to provide relief of heart ischemia. STEMI involves early invasive strategy of catheterization with angioplasty.
Medications:
Nitroglycerin (NTG) - It decreases blood pressure and dilates the blood vessels, increasing blood flow to the heart.
Morphine sulfate- Used as an analgesic.
Clot busting drugs (Thrombolytic) - They are used to dissolve the clots responsible for causing artery blockage and death of tissue. A thrombolytic drug needs to be given within 3 hours after the onset of symptoms. The standard thrombolytic drugs are recombinant tissue plasminogen activators or Rt-PAs such as Alteplase, Reteplase, and a newer drug Tenecteplase (TNKase).
Anti-platelet drugs
These drugs inhibit blood platelets from sticking together, thereby helping to prevent clots.
- Aspirin is the most common anti-clotting drug. Randomized trials have each demonstrated that, compared to placebo, aspirin reduces the risk of death or MI by more than 50% for patients presenting with UA/NSTEMI.

- Clopidogrel is a thienopyridine derivative that blocks the P2Y12 adenosine diphosphate (ADP) receptor on platelets. This action decreases platelet activation and aggregation, increases bleeding time, and reduces blood viscosity.
- Prasugrel is an irreversible P2Y12 ADP receptor antagonist that was recently approved by the US Food and Drug Administration.
- Ticagrelor is another new antiplatelet drug approved for patients with ACS.
- Glycoprotein IIb/IIIa Inhibitors are useful for patients at high risk. These powerful anti-platelet drugs include Abciximab, Eptifibatide, and Tirofiban.
Anticoagulant drugs thin the blood. They include:
- Unfractionated Heparin (UFH). The results of several randomized trials suggest that UFH is associated with lower rates of death or MI than is aspirin alone.
- Low Molecular-Weight Heparin (LMWH) for improved anticoagulation.
- Other intravenous anticoagulants include Bivalirudin, Enoxaparin, and Dalteparin.
Angiotensin-converting enzyme (ACE) inhibitors are useful for potential heart failure risk patients. They expand blood vessels and improve blood flow. They include Lisinopril, Benazepril, Captopril, Perindopril, Quinapril, and Ramipril.
Angiotensin receptor blockers (ARBs) help control blood pressure. They include Irbesartan (Avapro), and Losartan (Cozaar).
Statins lower the amount of cholesterol circulating in the blood. Statins include Atorvastatin (Lipitor), and Simvastatin (Zocor).
Calcium channel blockers such as Felodipine inhibit the contraction of both the myocardium and the vascular smooth muscle. The ACC/AHA guidelines recommend these agents for patients with persistent or recurrent symptoms after treatment with full-dose nitrates and β-blockers and for patients with angina.
Surgical:
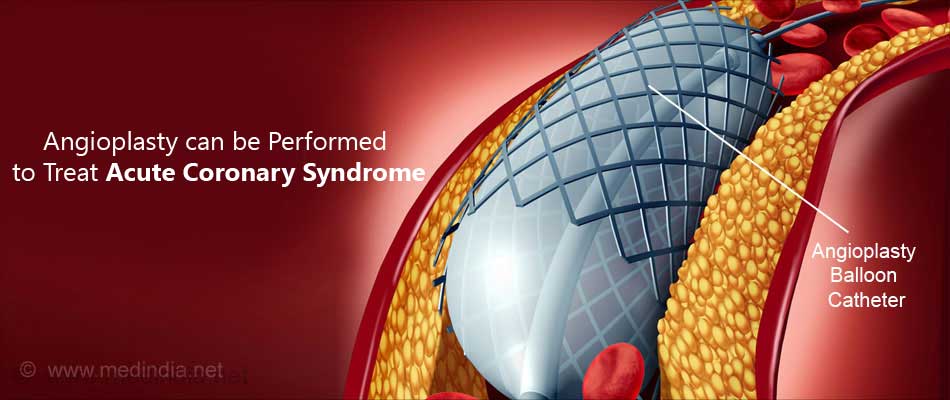
- Angioplasty (percutaneous coronary intervention) or PCI is the preferred emergency procedure for opening the arteries. Angioplasty should be performed promptly for patients with STEMI heart attack. In most cases, a stent [a miniature wire tube] is placed in the artery to keep it open after the angioplasty.
In certain cases of UA/NSTEMI, especially those who are considered high risk, an early invasive strategy may be followed which involves performing a cardiac catheterization and PCI within 4-24 hours of admission.
- Coronary artery bypass graft (CABG) surgery is sometimes used as an alternative to angioplasty. Segments of veins or arteries taken from other parts in the patient's body are used to reroute the blood. This surgery is often called “open heart surgery”.
What is the Prognosis of Acute Coronary Syndrome?
Patients with acute coronary ischemia are stratified into low and high risk groups depending on 3 scoring systems commonly used. This helps physicians to determine the outcome as well as decide whether to initiate early invasive treatment or go with conservative management.
The three systems include TIMI, GRACE and PURSUIT systems.
The TIMI system has been validated in several trials. It predicts outcome before discharge and at 14 days. However subtle discrimination is not possible in this system and it does not discriminate the effect of revascularization. However it is a simple and easy to use bedside tool.
The PURSUIT system predicts 30 day risk and uses vital signs measured initially at admission.
However more inclusive scoring systems need to be evolved. The current scoring systems have failed to include important factors such as anemia, extent of CAD C-reactive protein, and left ventricular ejection fraction (LVEF).