- Wang JD, Zhang JS, Xiong Y, Li J, Li XX, Liu X, Zhao J, Tsai FF, Vishal J, You QS, Huang Y, Wan XH. Congenital aniridia with cataract: case series. Wang et al. BMC Ophthalmology (2017) 17:115. DOI 10.1186/s12886-017-0503-6
- Improving molecular diagnosis of aniridia and WAGR syndrome using customized targeted array-based CGH - (https://doi.org/10.1371/journal.pone.0172363)
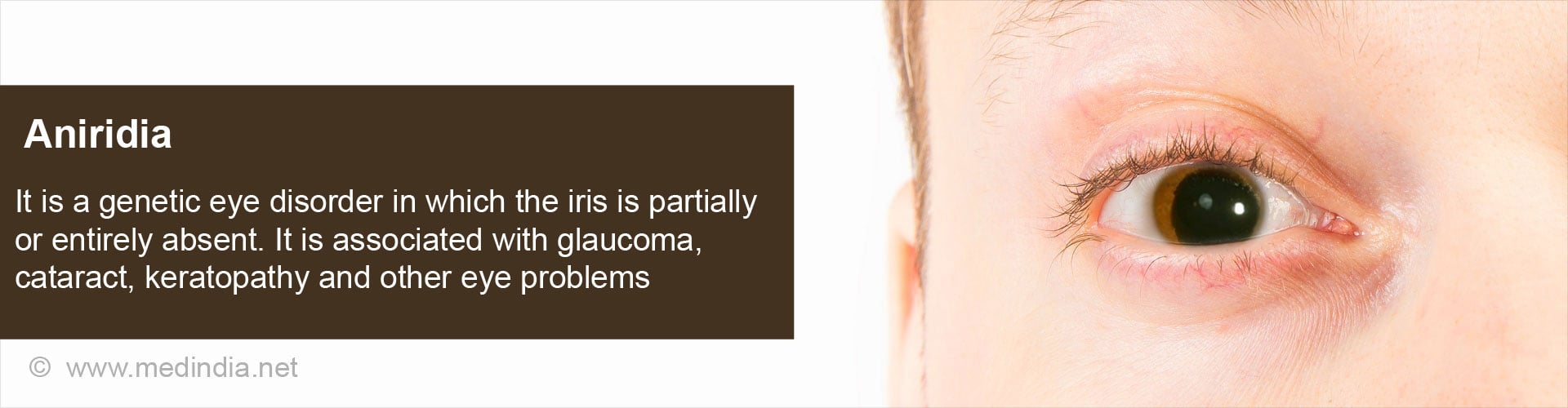
What is Aniridia?
Aniridia or congenital aniridia is an eye disorder marked by the partial or complete absence of the iris of the eye from birth. The iris is the colored disc that gives the eye its color. It has a small opening in the center called the pupil, through which light enters the eye.
Congenital aniridia affects both the eyes and is often also associated with other eye problems like glaucoma, cataract, keratopathy, nystagmus, disorders associated with the macula or the optic nerve and sometimes, retinal detachment.
How Common is Aniridia?
Congenital aniridia is an extremely rare condition, with an incidence as low as between 1: 64000 and 1: 100000.
What Causes Aniridia?
Congenital aniridia is a genetic disorder. It is found to be associated with a mutation in the PAX6 gene located on the short arm of chromosome 11 (11p13). The gene codes for a protein that is essential for the development of the parts of the eye.
The genetic disorder is inherited in an autosomal dominant pattern. Every person has a pair of each gene, one from either parent. A dominant form of inheritance means that even if one of the pair of the PAX6 gene is abnormal, the baby will suffer from aniridia. The presence of two copies of the defective gene can be serious, and can even result in death of the baby.
Some patients have an absent or defective ELT4 gene, which acts as a regulator of the PAX6 gene. These patients may have a normal PAX6 gene but still develop aniridia.
Aniridia can occur as a part of WAGR syndrome. WAGR stands for:
W - Wilms tumour
A - Aniridia
G - Genitourinary anomalies
R - Mental Retardation
Wilms tumor is a type of kidney cancer that usually affects children. Patients with WAGR syndrome have two missing genes, the PAX6 gene and the WT1 gene.
Aniridia is also associated with other genetic syndromes like Gillespie syndrome, and Peters anomaly.
Some cases do not have a family history and the aniridia may appear sporadically. Children with sporadic aniridia have a 30% chance of developing Wilm’s tumor.
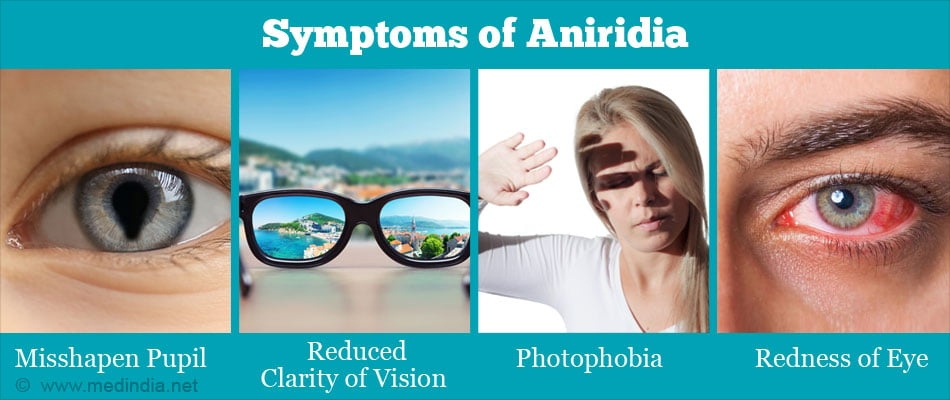
What are the Symptoms of Aniridia?
Congenital aniridia affects both the eyes; sporadic cases may affect only one eye. The partly or completely missing iris may result in the following:
- An eccentric or misshapen pupil
- Aesthetic problems
- Reduction in visual acuity or clarity of vision
- Photophobia or increased sensitivity to light
Other associated features depend on the part of the eye affected. The parts of the eye affected in aniridia include:
Cornea: The cornea is the transparent dome at the center of the eye through which light enters the eye. Disease of the cornea is referred to as keratopathy. In patients with aniridia, the cornea may thicken and develop blood vessels, first in the periphery, which then progresses to the center. Erosions and ulcers can occur, due to which the cornea may turn opaque resulting in blindness. The symptoms of corneal disease may include:
- Dry eye with reduced tear formation and abnormal tear film
- Redness of eye
- Photophobia or increased sensitivity to light
- Reduced visual acuity
- Blepharospasm or tight eyelid muscles
- Increased risk of bacterial infection
- Perforation of the eye
- Blindness
Lens: The lens may get clouded resulting in cataract. Unlike the usual cases of cataract, the cataract in patients with aniridia appears early, often within the first two decades of life. The lens may also get displaced from its location, which is referred to as subluxation of the lens.
Retina, macula and optic nerve: The retina is the light sensitive layer of the eye, with the macula being the area responsible for the central vision. The optic nerve carries signals from the eye to the brain. Conditions associated with aniridia that affect the retina, macula or the optic nerve reduce vision but may be difficult to diagnose due to associated defects like cataract and keratopathy. Retinal tears and retinal detachment may also occur. An increase in the pressure within the eye occurs due to a problem with the drainage of the intraocular fluid, which can damage the optic nerve. This is referred to as glaucoma, and occurs in about 75% of cases. It presents in older children or during adolescence
In addition, the following may be noted:
- Nystagmus or involuntary movement of the eyes
- Strabismus or squint
How do you Diagnose Aniridia?
Aniridia is diagnosed based on several tests. However, it may not be always possible to carry out all the tests in children, and it may be difficult to examine the deeper structures in the presence of corneal and/or lens opacities. Some tests that are used to diagnose aniridia include the following:
- Examination of visual acuity: The visual acuity is measured using the Snellen chart.
- Ophthalmoscopy: Ophthalmoscopy helps to examine the inner structures of the eye. The eye may or may not be dilated for the examination.
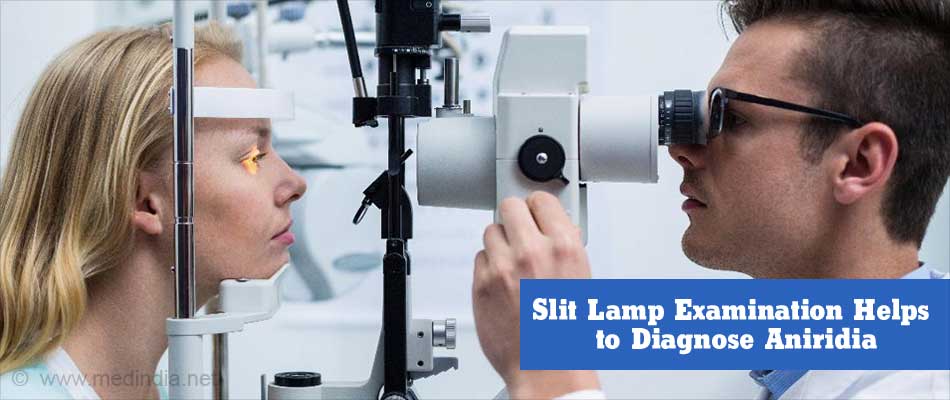
- Slit lamp examination: The slit lamp helps in the examination of the eye structures like the cornea, the anterior chamber (the space between the iris and lens and the cornea), iris, lens and the vitreous humor (the thick gel-like fluid behind the lens). With special lenses, deeper structures like the optic nerve and the retina can be examined. The patient will be asked to seated and place the chin on a chin rest of the instrument. The ophthalmologist will sit on the opposite side and examine the eye. He/she may put eye drops to dilate the eye, numb the eye or temporarily stain the cornea for better visualization. The slit lamp can also be used to examine the drainage angle, between the cornea and the iris (gonioscopy).
- Tonometry: Tonometry is the measurement of the pressure within the eyeball. It is done with the help of special instruments. The eyes are usually numbed with a local anesthetic before the procedure.
A family history should also be determined. The parents should also be examined for the presence of any eye defect. Genetic testing can be carried out to confirm the presence of a genetic defect. Children with genetic changes that predispose to Wilms tumor should undergo regular ultrasounds to detect the tumor at the earliest- roughly every 3-6 months till 10 years of age, and annually up to the age of 16 years.
How do you Treat Aniridia?
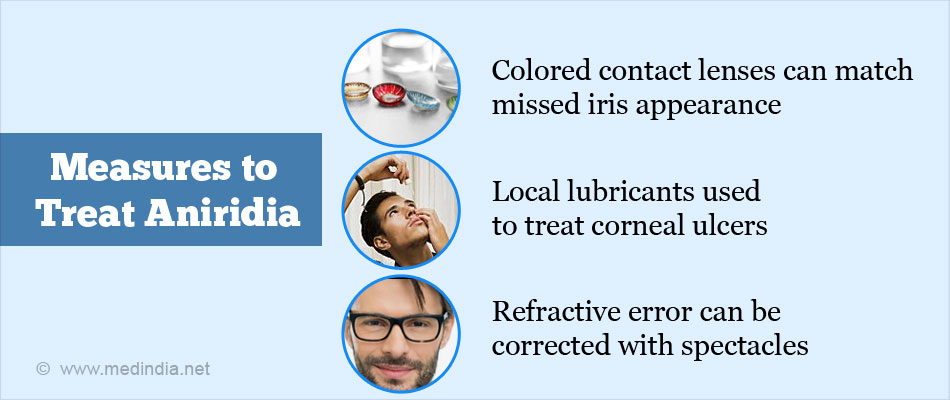
Aniridia requires treatment of other associated eye problems as well in addition to the absent iris. Treatment measures include the following:
- The cosmetic effect of the missing iris can be improved by using colored contact lenses. Several patients do not tolerate contact lenses over prolonged durations. Another option is the implantation of the black diaphragm intraocular lens into the eye to cover the defect. Dark glasses may be advised to protect the eye from photophobia prior to surgery.
- Mild corneal disease is treated with artificial tears without preservatives. Local lubricants and antibiotics are used for corneal ulcers. Autologous serum and amniotic membrane grafts, or transplantation of limbal stem cells (cells that help to regenerate the surface corneal layer) may be used for more serious cases. An artificial corneal prosthesis may be implanted in patients with treatment failures.
- The increase in intraocular pressure (glaucoma) is treated by surgery.
- Any refractive error is corrected with spectacles.
- Cataract and squint require surgical treatment.
- Genetic counselling should be offered to families with a genetic defect or a genetic syndrome.