- A Review of Cardiogenic Shock in Acute Myocardial Infarction - (https://www.ncbi.nlm.nih.gov/pmc/articles/pmc2774583/)
- Cardiogenic Shock - (http://circ.ahajournals.org/content/117/5/686)
What is Cardiogenic Shock?
Cardiogenic shock occurs as a result of reduced pumping ability of the suddenly weakened heart due to various causes, such as damage to the muscles of heart from a severe heart attack; this results in insufficient blood being pumped out and not meeting the body’s requirements. Since the heart is not able to pump out all the venous return coming to it, it leads to the congestion of the lungs and viscera, and hence the condition is called congested shock.
The condition is a medical emergency and is fatal if not treated right away. It is a stage of end organ hypoperfusion which sets in due to the cardiac failure. It occurs in five to eight percent of the people admitted due to ST-elevation myocardial infarction. It is the most common cause of death in hospitalization due to heart attack.
What is the Pathophysiology of Cardiogenic Shock?
- In cardiogenic shock, both impaired contraction of the heart muscle (systolic dysfunction) and impaired ventricular filling (diastolic dysfunction) occur.
- Most of the patients have multiple vessel coronary artery disease with decreased blood supply (ischemia) to the heart muscle (myocardium) resulting in its death (necrosis).
- The impaired left ventricular filling causes back flow of blood into the lungs resulting in pulmonary edema and impaired gas exchange leading to low oxygen levels in the blood (hypoxemia).
- The loss of viable heart muscle further causes heart muscle dysfunction aggravating the ischemia of the myocardium.
- The resulting decreased cardiac output and blood flow to various vital organs leads to multiple organ dysfunction which may result in death.
- Three organs of vital importance are the brain, heart, and kidneys. Reduced blood flow to the brain can result in altered sensorium and coma. Heart dysfunction and reduced cardiac output further aggravates the hypoperfusion state. Reduced blood flow to the kidneys reduces urinary output and ultimately kidney failure.
- Additionally, ischemia of heart muscle followed by restoration of blood flow can cause systemic inflammation and sepsis due to relocation of intestinal bacteria and bacterial toxins contributing to increased mortality.
What are the Causes of Cardiogenic Shock?
- Myocardial infarction or heart attack with left ventricular failure involving more than forty percent of the left ventricular myocardium forms the commonest cause of cardiogenic shock.
- Factors which complicate myocardial infarction and precipitates cardiogenic shock include rupture of papillary muscle and the inter ventricular septum.
- Aortic dissection: excessive blood loss my lead to extreme hypoperfusion and precipitate cardiogenic shock
- Mitral and aortic stenosis: again, the stenosed valve causes reduced blood flow to the body and the hypoperfusion leads to shock
- Congestive heart failure: is in itself a state of hypoperfusion where enough blood is not pumped to meet the body’s needs.
- Severe valvular dysfunctions like acute aortic regurgitation, acute mitral regurgitation also have an adverse effect on the amount of blood pumped out by the left ventricle per minute.
- Acute massive pulmonary embolism: causes a block in the blood vessels of the lungs, thereby decreasing the amount of blood entering the heart and eventually decreaseing the amount of blood that gets distributed in the body, and hence creates a state of hypoperfusion.
- Pericardial tamponade: In a massive cardiac tamponade, fluid is filled in the membranes covering the heart, and in turn compressing it; the heart is thus unable to pump out adequate blood to the body, and hence creating hypoperfusion.
- Cardiac arrhythmias.
- Toxic states of heart.
- Dilated cardiomyopathy.
- Cardiac tumours.
- Myocarditis.
What are the Signs and Symptoms of Cardiogenic Shock?
Decrease in the tissue and organ blood flow leads to multiple organ system failure and the signs and symptoms are categorized organ wise as follows:
- GIT: Hemorrhage is seen
- Skeletal muscles:
- Hyperkalemia: Increased potassium levels in the blood
- Lactic acidosis: Decreased tissue perfusion leads to reduced oxygenation and anaerobic cycle of energy production sets in the body, where lactic acid is the end product of glucose, which is used to break down to release energy for bodily needs. Accumulation of lactic acid leads to lactic acidosis and is harmful for the body
- Skin:
- Cold and clammy skin
- Cyanosis: it is the bluish discoloration of the skin due to decreased oxygenation
- Gangrene: is a life threatening condition set in as result of necrosis caused by potentially fatal reduced oxygenation and blood supply
- Brain:
- Confusion and irritability
- Stupor
- Tachypnea: Increased rate of breathing to compensate for the reduced oxygenation
- Cheyne-Stokes breathing: it is an abnormal pattern of breathing seen in patients with heart ailments
- Coma
- Kidneys:
- Oliguria: decreased urine output <30 mL/ hour and it is an indicator of impending kidney failure
- Acute Tubular Necrosis: it is an injury to the kidney which is caused by the lack of oxygen and blood supply to kidneys and can lead to the establishment of renal failure if not treated on time
- Hyperkalemia
- Lactic acidosis
- Heart:
- Tachycardia: increased heart rate > 100/ minute
- Thready pulse
- Angina: tight squeezing and constricting chest pain
- Pulmonary edema
- Arrhythmias: irregularity in the rhythm of heart beat
- Hypotension: decreased systolic Blood pressure <90 mmHg
How do you Diagnose Cardiogenic Shock?
1. Diagnosis is made by some typical clinical parameters
- Left ventricular systolic pressure <90 mmHg for at least 30 minutes
- Heart rate >100 beats/ minute
- Urine output <30 mL / hour
- Reduced cardiac output on echocardiogram
- Elevated left ventricular filling pressure measured by Doppler echocardiography
2. Laboratory tests
- Arterial blood gas measurements show reduced oxygenation of blood
- Base deficit increase correlates with the intensity of the shock and should be monitored to assess the clinical response following resuscitation
- Elevated serum lactate levels is associated with a poor prognosis and high mortality rates
- Cardiac enzymes such as Troponins T and I are measured to diagnose ischemic damage and injury to heart muscle
- Liver and kidney functions are assessed to determine the functional status of these organs
- Blood count may show increased white cell count (leucocytosis) and low platelet counts (thrombocytopenia) indicating underlying sepsis
3. The diagnosis is confirmed by the following:
- Electrocardiography (ECG): An ECG may show evidence of myocardial ischemia such as ST-segment elevation, ST-segment depression, or Q waves. A normal ECG however does not rule out presence of ischemia.
- Echocardiography: It is necessary to perform an echocardiogram to find out the cause of the cardiogenic shock. It may reveal akinetic or dyskinetic areas of heart muscle and valvular pathology. Left ventricular ejection fraction (LVEF) can also be measured.
- Pulmonary artery (PA) catheterization: Pulmonary artery catheter is a balloon tipped catheter that is inserted in the artery carrying away the blood from the heart to the lungs. It was initially used in the management of myocardial infarction. It measures the pressure in the artery going into lungs from the heart, oxygen saturation in the blood, blood pumped out by the left ventricle per minute, blood pumped out by the left ventricle per heartbeat, and the pressure in the capillary network of lungs.
How do you Treat Cardiogenic Shock?
The medical treatment of cardiogenic shock can be monitored for its efficacy by measuring the changes in cardiac output and left ventricular filling pressure, both before and after the administration of various vasopressor, inotropic, and volume expansion drugs and altering the dosage and frequency accordingly.
Treatment of shock is discussed under the following headings:
- Patient monitoring
- General measures
- Drug therapy
- Reperfusion therapy
- Surgical therapy
1. Patient monitoring
- Clinical monitoring of pulse, blood pressure and respiration
- Electrocardiographic monitoring of cardiac rate, rhythm, and arrhythmias
- Measure arterial blood gases and pH for correction of acidosis and hypoxia
- Pulmonary capillary wedge pressure monitoring
- Monitoring hourly urinary output
2. General measures
- Care of the skin, airway, bowel and bladder, and nutrition as the patient requires prolonged hospitalization
- Relieve pain by intravenous morphine sulfate

- Put the patient in a propped up position, which is the most comfortable position to relieve shortness of breath
- Correction of hypoxia is done by oxygen face masks or nasal prongs, and if necessary, by intubation and mechanical ventilation devices
- Acidosis is treated with intravenous sodium bicarbonate infusion
3. Drug Therapy
Drugs must be used only after correcting the volume deficit and heart rate. They act by increasing the cardiac output and allow better perfusion and redistribution of blood flow to vital organs like kidneys, heart and brain. The drugs used are:
- Dobutamine
- Combination of dopamine and dobutamine
- Vasopressin
- Vasodilation by nitroglycerine and nitroprusside
4. Reperfusion Therapy
Cardiogenic shock can be both treated and prevented by very early re-perfusion therapy for myocardial infarction. Early revascularization for cardiogenic shock improves survival drastically.
Drugs used are:
- A combination of aspirin and heparin should be given
- Clopidogrel may also be used
- Thrombolytics are agents that dissolve clots and restore blood flow to the heart. These are generally given when emergency heart catheterization facilities are not available
Medical Procedures - these aim to restore blood flow to the heart and include
- Angioplasty and stenting - If a block in the coronary vessel is found, a long thin tube (catheter) with a special balloon is inserted via the artery in the thigh and once in position, the balloon is inflated to open up the blockage. A metal stent may be placed in the artery to maintain its patency. In many cases the stent is coated with medication that releases slowly and helps to keep the vessel open.
- Intra-aortic balloon counterpulsation (IABP) - A balloon is placed in the major vessel, the aorta. It inflates when the heart relaxes and deflates when the heart contracts. It improves the perfusion to both the heart muscles as well as to the entire body. It increases the left ventricle performance by alternating inflation and deflation.
5. Surgical therapy
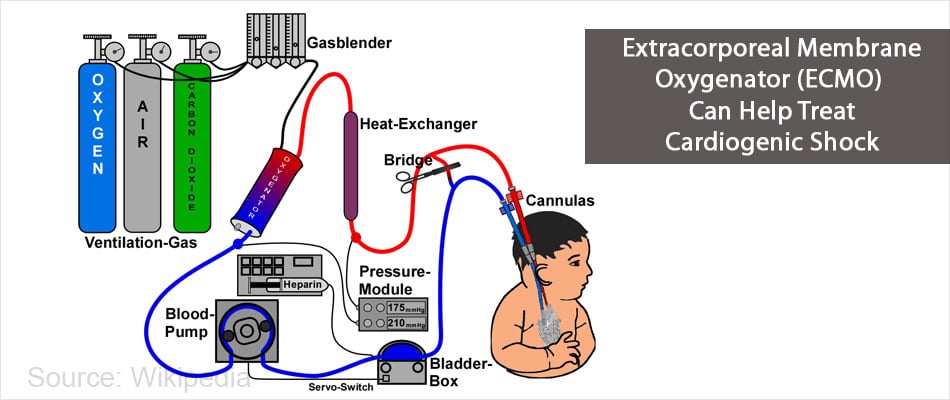
Circulatory assist devices: these may be beneficial in selected cases of cardiogenic shock. The various modalities included are:
- Partial cardiac bypass (left ventricle assist devices)
- Extracorporeal membrane oxygenator (ECMO)
Coronary artery Bypass surgery – The surgery is done to restore blood flow in a blocked coronary vessel. Grafts from saphenous vein in the leg or the artery on the chest wall are taken and attached to the coronary vessel beyond the block. The distal end of the graft is attached to the aorta.
Other conditions requiring surgery
It aims to correct the underlying cause. It is indicated in following cases
- Ruptured papillary muscle
- Acute mitral regurgitation
- Rupture of the interventricular septum
- Acute aortic regurgitation
- Aortic dissection
- Acute massive pulmonary embolism
How do you Prevent Cardiogenic Shock?
The ideal way to prevent cardiogenic shock is to prevent a heart attack, which could be achieved by the following measures:
- Adopt a healthy lifestyle
- Avoid the consumption of cigarette, tobacco, recreational drugs, alcohol, and caffeine
- Practice meditation and yoga to reduce stress
- Maintain a healthy weight; being obese contributes to other risk factors
- Eat a healthy and a balanced diet. Eat a diet low in cholesterol and fats
- Diabetic patients must maintain their sugar levels in the normal range and take the medicines regularly
- Manage your high blood pressure, take antihypertensives regularly and eat a low salt diet
- Avoid stress and hectic schedules
- Maintain a healthy sleep pattern
- Inspite of these preventive measures, if an acute myocardial infarction occurs, immediate hospitalization and administration of early revascularization and reperfusion therapies might prevent the advent of cardiogenic shock